From Prescription Pad to EHR: How ePrescriptions Became the Default
Paper prescriptions had their quirks — smudged ink, illegible handwriting, and the occasional frantic pharmacy call to confirm if that was “20mg” or “200.” But they stuck around for decades because they were simple. No logins, no integrations, no standards. Just a signature and a stamp.
Then came the push to digitize. First, through incentive programs and later through necessity, providers began writing prescriptions inside EHRs and sending them directly to pharmacies. It wasn’t a flashy change. But it quietly rewired one of the most routine actions in care delivery: getting a patient the medication they need.
ePrescriptions (or eRx) today aren’t just digital versions of paper scripts. They tap into drug databases, check insurance coverage, catch interactions, and route instructions to pharmacies in real time. What looks like a simple click carries a lot more behind the scenes.
In this blog, we break down what actually happens between the moment a prescription is written and the moment it’s ready for pickup.
Step One: Where It All Starts – The Point of Care
Every prescription begins with a clinical decision. Maybe the patient has a recurring infection. Maybe they’re recovering from surgery. Or maybe they just got diagnosed with hypertension. The physician’s job is to decide what medication makes sense, but today, that decision doesn’t live in isolation.
At the point of care, most providers work inside an EHR or an ePrescribing module. They select the drug, dosage, route, and instructions — but it’s more than just typing it in. The system may pull up formulary details, medication history, or real-time alerts if something looks off. For example:
- A pop-up might warn: “This drug interacts with one the patient’s already on.”
- Or: “This isn’t covered by their plan, but the generic is.”
Some systems go further, suggesting alternatives that are clinically equivalent but cheaper or more accessible. These nudges matter — not just for clinical accuracy, but also to avoid last-minute pharmacy callbacks and patient frustration.
So, while it might feel like “just writing a script,” this first step is actually the foundation. It’s where medical judgment, system intelligence, and patient context start working together — long before anything reaches the pharmacy.
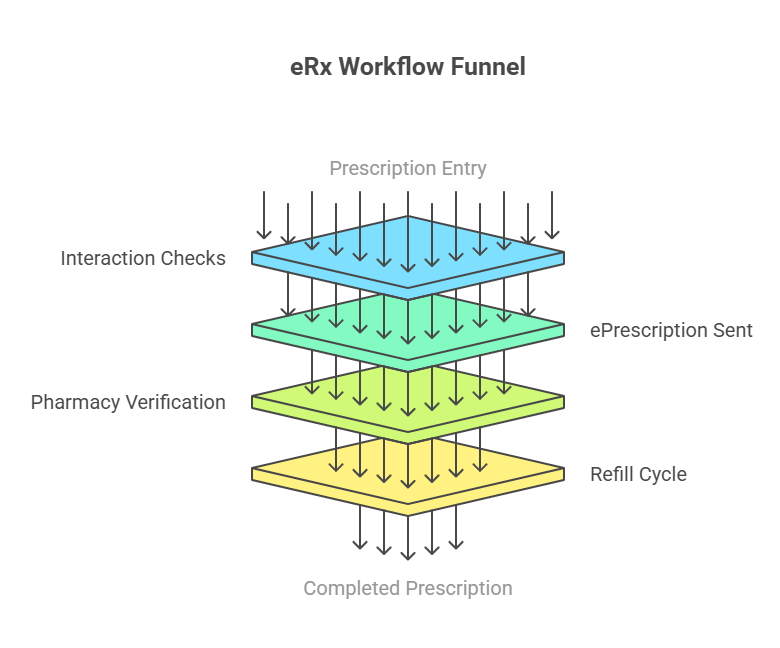
Step Two: What Happens Before the Prescription Leaves the EHR
Once the provider selects a medication, the system doesn’t immediately send it off to the pharmacy. Instead, it initiates a series of checks to ensure the prescription is appropriate and covered:
1. Medication History Retrieval
The system queries pharmacy benefit managers (PBMs) and pharmacies to retrieve up to 12 months of the patient’s medication history. This data helps identify potential issues like duplicate therapies or drug interactions. Such medication history retrieval is a critical safety check supported by national eRx networks.
2. Formulary and Eligibility Verification
The system checks the patient’s insurance formulary to confirm if the prescribed medication is covered. If not, it may suggest alternatives that are covered, such as generic versions. This step helps prevent delays at the pharmacy due to coverage issues.
3. Real-Time Benefit Checks
Some systems provide real-time information about the patient’s out-of-pocket costs for the prescribed medication. This transparency allows providers to discuss cost-effective options with patients, potentially improving adherence.
By conducting these checks upfront, the system aims to minimize issues that could arise later, ensuring a smoother experience for both the provider and the patient.
Step Three: Sending the Prescription — But Not Like an Email
Once everything’s finalized — the drug, dosage, instructions, and insurance coverage — the system doesn’t just “send” the prescription. It transmits it through a secure, real-time, standards-based network. This is where ePrescribing shifts from clinical action to technical execution.
Most providers in the U.S. route prescriptions through national eRx networks like Surescripts, which processed over 2.5 billion ePrescriptions in 2023, including those for controlled substances. This scale reflects not just high adoption, but the system’s role as critical infrastructure — connecting over a million prescribers, 65,000 pharmacies, and multiple EHR platforms.
But volume alone doesn’t ensure safety. What makes this work is the NCPDP SCRIPT Standard, developed by the National Council for Prescription Drug Programs. It’s a structured data format — not a PDF or static file — that ensures every field (drug name, strength, SIG, refill instructions, identifiers, pharmacy location) is machine-readable and validated.
Before reaching the pharmacy, the ePrescription may also pass through a transaction hub that checks for formatting errors, routing mismatches, or missing data. This step helps prevent breakdowns in communication and ensures the pharmacy system receives a clean, actionable order.
Once received, the pharmacy system sends back a digital confirmation — a status message indicating successful delivery, often including timestamps and IDs. If anything fails (e.g., invalid NPI, pharmacy closed), the system notifies the provider instantly, prompting a correction.
This bidirectional loop, with structure, validation, and acknowledgment, makes ePrescribing dramatically more reliable than paper or fax-based processes. It’s not just about speed; it’s about confidence that the right order reaches the right hands, every time.
Step Four: The Pharmacy Fulfills the Order
Once the e-prescription reaches the pharmacy, the real work begins. The pharmacy system parses the structured data — medication name, dosage, instructions, and patient details — and prepares the medication for dispensing.
This step involves several key actions:
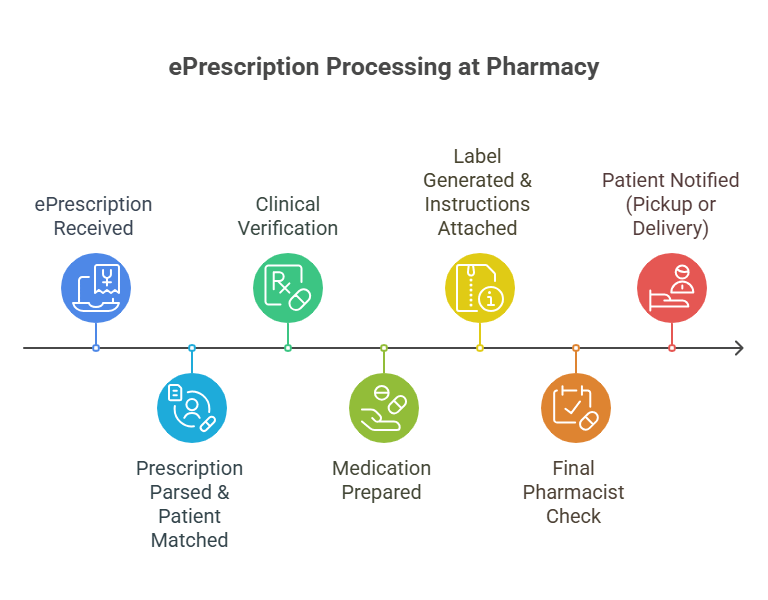
- Verification: The pharmacist reviews the prescription for accuracy, cross-checking it with the patient’s profile, any known allergies, and current medications already on file. If discrepancies are found, such as a high-risk interaction, the pharmacy may contact the prescriber for clarification before proceeding.
- Preparation: After verification, the pharmacy staff prepares the medication according to the prescribed dosage and form. For specialty drugs or compounded medications, this may involve additional checks, inventory pulls, or technician involvement.
- System Matching & Labeling: eRx data flows into the pharmacy management system, linking to the correct patient record. Labels, instructions, and counseling notes are auto-generated based on the structured prescription data, minimizing manual entry and reducing transcription errors.
- Notification: Once ready, the pharmacy sends a text, email, or app alert to the patient for pickup. In some cases — especially mail-order or specialty pharmacies — delivery is coordinated directly with the patient or caregiver.
With structured, electronic prescribing, the chance of misreading handwritten notes is eliminated. According to a study published by the Journal of the American Medical Informatics Association, e-prescribing systems can reduce medication errors by up to 80% compared to handwritten prescriptions.
Moreover, because most large pharmacies are fully integrated with eRx networks, fulfillment turnaround times have shortened, and pharmacy workflows have become more predictable, benefiting both staff efficiency and patient satisfaction.
Step Five: Refill Management & Renewals
Prescriptions don’t always end with the first fill. For chronic conditions like diabetes, asthma, or hypertension, patients rely on timely refills and renewals to maintain consistent therapy. Poor coordination here can lead to treatment gaps, increased health risks, and unnecessary provider workload.
Modern ePrescribing systems are built to handle this continuity. Once a prescription is on file, the pharmacy system tracks when a refill is due. Many pharmacies now trigger automated refill reminders through SMS, app notifications, or email, helping patients avoid missed doses — a common cause of preventable readmissions.
When a prescription runs out of authorized refills, the system can automatically generate a renewal request from the pharmacy to the provider. This eliminates the need for phone calls or faxes, instead using the same structured standards (like NCPDP SCRIPT’s renewal message format) to route the request through the eRx network.
On the provider’s end, renewals show up in their EHR queue. They can approve, modify, or deny them with just a few clicks. This reduces administrative back-and-forth, especially for primary care practices that receive dozens of refill requests per day.
Some systems also offer patient-initiated renewals via portals, where patients can view their current prescriptions and request refills without having to contact the office. For providers, this translates to more manageable workflows. For patients, it means fewer delays in access to medications they’ve already been stabilized on.
Effective refill and renewal workflows are often where ePrescribing systems prove their value, not just in new prescriptions, but in reducing the friction of long-term medication management.
Section Six: Compliance and Security in ePrescribing
With sensitive patient data and controlled substances involved, ePrescribing isn’t just about convenience — it’s also a matter of regulatory compliance and system integrity.
In the U.S., ePrescribing must comply with several federal regulations, most notably the DEA’s Electronic Prescriptions for Controlled Substances (EPCS) rule. This rule mandates that prescriptions for Schedule II–V substances be transmitted electronically using certified systems that support multi-factor authentication, audit trails, and tamper-resistant records.
To meet these requirements, certified eRx platforms include safeguards such as:
- Two-factor authentication (2FA) for prescribers at the point of signing
- Audit logs that track every action, from prescription entry to renewal approval
- Digital signing and identity proofing, verified through certified credential service providers (CSPs)
For general prescribing, HIPAA sets the bar for protecting patient health information (PHI). eRx data travels over encrypted channels, often through intermediaries like Surescripts, which maintain their own network security certifications and uptime guarantees.
The use of the NCPDP SCRIPT Standard adds another layer of safety, not just in terms of interoperability, but also in minimizing ambiguity. Unlike free-text messages, structured eRx records eliminate misinterpretation and reduce the risk of fraud.
State laws also play a role. As of 2024, nearly all U.S. states have adopted mandatory ePrescribing for opioids and other controlled substances to combat opioid abuse and close diversion loopholes.
Compliance isn’t just a checkbox — it’s what enables trust in the entire prescribing chain. For healthcare organizations, using a compliant eRx system reduces legal exposure and positions them for alignment with federal incentive programs and payer requirements.
Section Seven: Benefits of ePrescribing for Providers, Pharmacies, and Patients
Beyond faster prescriptions, the real value of ePrescribing shows up in the day-to-day experience of care delivery. When done right, it creates clarity, reduces repetition, and improves outcomes across the board.
For Providers
- Fewer interruptions: With real-time formulary checks and renewal workflows built into the EHR, providers spend less time fielding calls from pharmacies.
- Improved documentation: Every prescription sent is logged, time-stamped, and auditable, which supports both clinical tracking and regulatory compliance.
- Better clinical decisions: Access to medication history, allergy alerts, and drug interaction warnings helps avoid errors at the point of prescribing.
For Pharmacies
- Streamlined fulfillment: Structured data means fewer manual entries. Pharmacists receive all necessary details in a format that integrates directly into their dispensing system.
- Reduced clarification calls: Legibility issues and missing information are nearly eliminated, freeing up pharmacy staff to focus on verification and patient counseling.
- More predictable workflows: Automated acknowledgments, renewals, and refill tracking help pharmacies manage volume more efficiently.
For Patients
- Shorter wait times: Prescriptions arrive at the pharmacy electronically, often before the patient even leaves the clinic.
- Lower out-of-pocket costs: Real-time benefit tools help providers choose affordable options, improving medication adherence.
- Fewer missed doses: Refill reminders and renewal automation reduce the chances of running out of necessary medications.
When each step of the process — from prescribing to fulfillment — is digitally coordinated, the experience improves for everyone involved. ePrescribing isn’t just a convenience layer; it’s part of a safer, smarter healthcare infrastructure.
Conclusion: Connecting the Dots in ePrescribing
What looks like a simple act — sending a prescription — is actually a layered process involving clinical judgment, data validation, secure transmission, pharmacy coordination, and long-term medication tracking. Each step plays a role in making medication management safer, faster, and less prone to error.
As healthcare moves toward more connected, standards-driven systems, ePrescribing has become a core function, not just for compliance, but for quality of care.
At Nalashaa, we help healthcare organizations modernize the systems behind these experiences. Whether it’s building custom EHR modules, integrating eRx workflows, supporting EPCS compliance, or streamlining refill management, our healthcare software solutions are designed to simplify what shouldn’t be complicated.
If you’re working on improving your digital prescribing capabilities or embedding smarter pharmacy workflows into your platform, we build for that.
Reach out at info@nalashaa.com to start the conversation.
Latest posts by Priti Prabha (see all)
- ONC HTI 1 Final Rule and Certified APIs: A Complete Guide - February 19, 2026