Healthcare has never lacked data or expertise — it has struggled with connection. A patient might see three specialists, visit two labs, and interact with multiple administrative systems, yet their information often lives in disconnected silos. This fragmentation leads to duplication, higher costs, and delayed care decisions.
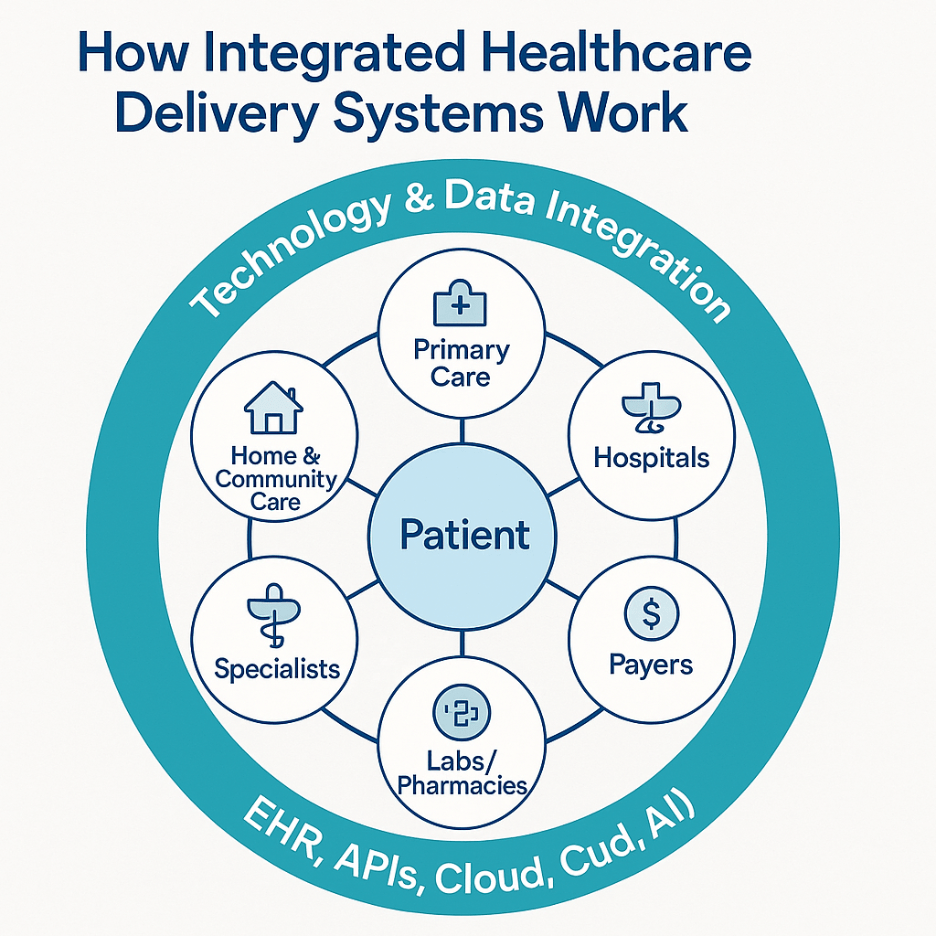
To overcome this, healthcare leaders are turning into integrated healthcare delivery systems — networks that align hospitals, clinics, payers, and digital platforms under one unified model. Integration represents the next stage in healthcare evolution: where information moves freely, care teams collaborate across boundaries, and the patient becomes the consistent center of every interaction.
What Is an Integrated Healthcare Delivery System?
An integrated healthcare delivery system (IHDS) is a coordinated network of healthcare organizations that provides a continuum of care from primary to tertiary services under a shared structure. Instead of operating as isolated entities, these systems combine providers, hospitals, laboratories, pharmacies, and insurers through shared governance, information, and accountability.
The objective is clear: deliver value-based care, where the focus shifts from volume of services to quality of outcomes. This means better patient experiences, reduced redundancies, and financial models tied to efficiency rather than procedure counts.
Integration also redefines the patient’s journey. A person moving from preventive care to rehabilitation can now transition seamlessly because all their health data, clinical notes, and billing information stay synchronized.
Why Integration Matters in Modern Healthcare
Healthcare fragmentation is not just inconvenient — it’s costly and unsafe. Studies show that redundant lab tests and miscommunication between providers account for billions in annual healthcare waste. Even more concerning is the human impact: inconsistent treatment plans, medication conflicts, and diagnostic delays.
An integrated healthcare delivery system addresses these issues through:
- Coordinated Care: Each provider sees the same patient record, reducing duplication and improving accuracy.
- Continuity: Information follows the patient, ensuring smoother transitions between facilities.
- Accountability: Shared outcomes encourage proactive, preventive care rather than reactive treatment.
- Efficiency: Unified systems lower administrative overhead and optimize resource use.
According to the World Health Organization (WHO), integrated care is key to achieving equitable and sustainable health outcomes. It ensures that “people receive a continuum of health promotion, disease prevention, diagnosis, treatment, and rehabilitation services through coordinated action across different levels of the system.”
Core Components of an Integrated Healthcare Delivery System
Every IHDS has four layers that define how coordination happens: clinical, financial, informational, and organizational integration. Together, these layers ensure both care and infrastructure operate in sync.
1. Clinical Integration
At the heart of integration lies teamwork. Physicians, specialists, and care managers operate under shared protocols and treatment pathways. This creates consistency in diagnosis and therapy, especially for chronic disease management. Clinical integration also supports multidisciplinary care; a patient recovering from a cardiac event might have their cardiologist, physiotherapist, and nutritionist working from the same plan.
2. Financial Integration
Financial alignment ensures that incentives support outcomes, not activity. Hospitals and payers adopt value-based contracts, bundled payments, or shared risk models. This encourages prevention, early intervention, and efficient use of resources.
3. Information Integration
A hallmark of integrated healthcare delivery systems is the free flow of data. Electronic Health Records (EHRs) form the backbone, enabling providers to access complete patient histories. Health Information Exchanges (HIEs) and interoperability standards such as HL7 and FHIR further connect different IT systems, ensuring data moves securely and in real time.
4. Organizational Integration
Behind every successful IHDS is aligned governance. Hospitals, outpatient centers, and administrative units share leadership strategies and key performance metrics. This ensures every part of the system works toward common goals — patient satisfaction, operational efficiency, and clinical quality.
How Technology Powers Integration
Technology is both the enabler and the glue that holds an integrated system together. Without digital connectivity, coordination would still depend on manual processes, faxed reports, and delayed communication.
Let’s explore how technology strengthens integration across layers:
| Technology | Role in Coordination |
| EHR/EMR Systems | Centralize medical records, ensuring providers have access to accurate data at every point of care. |
| Interoperability APIs | Allow seamless exchange of patient data between labs, hospitals, and insurers. |
| Analytics Platforms | Enable data-driven decisions for population health management and risk stratification. |
| Telehealth & Patient Portals | Extend engagement beyond facilities, ensuring continuous monitoring and communication. |
| Cloud Infrastructure | Supports scalability and secure storage of health data across organizations. |
| AI and Predictive Tools | Identify care gaps, forecast readmissions, and improve diagnostic accuracy. |
Example: When a patient is discharged from a hospital, their records automatically update in the primary physician’s EHR. This triggers follow-up scheduling, medication reminders, and remote monitoring alerts — all without manual handoffs.
This automation reduces friction across departments, minimizes data loss, and enhances the patient’s experience.
Studies by the National Institutes of Health (NIH) highlight how AI-driven coordination and data integration are improving clinical efficiency and decision accuracy in hospital networks. The fusion of interoperability and intelligence is making coordinated care both scalable and measurable.
Real-World Examples of Integrated Delivery Models
Some of the most successful integrated systems already operate at scale, proving that the model works both clinically and financially.
Kaiser Permanente (United States)
Perhaps the most recognized IHDS, Kaiser integrates its hospitals, health plan, and physician groups under one organization. This closed-loop model ensures aligned incentives, shared data, and population health management. Their integrated EHR system enables real-time communication between doctors and patients, resulting in fewer readmissions and better chronic care outcomes.
Mayo Clinic Health System (United States)
Mayo operates multiple facilities and specialties through shared governance and unified patient records. Every physician can access a complete view of a patient’s health journey, allowing collaborative decision-making and personalized care.
NHS Integrated Care Boards (United Kingdom)
The UK’s National Health Service established Integrated Care Boards (ICBs) to manage regional healthcare networks. These boards coordinate hospitals, community health, and social services, emphasizing preventive health and shared accountability.
Each example underscores one principle: integration succeeds when data, incentives, and care pathways align under a common goal — better health outcomes.
Challenges in Building Integrated Healthcare Systems
While the benefits of integrated healthcare delivery systems are undeniable, achieving them is far from easy. True integration demands more than connected software; it requires cultural change, aligned incentives, and long-term commitment from all stakeholders.
Here are some of the most common challenges healthcare leaders face on the path to integration:
1. Interoperability Gaps
Even as interoperability standards like FHIR and HL7 gain traction, many healthcare organizations still operate on legacy systems. These systems were never designed to exchange data easily, leading to incompatible formats and duplicated information.
Without seamless data exchange, the “integration” remains partial — administrative teams still re-enter patient data manually, and providers lack a complete view of clinical history.
This challenge is often addressed by implementing healthcare data integration services that unify systems and create a single source of truth across care settings.
2. Governance and Accountability
Integration blurs the traditional lines between organizations. Hospitals, independent practices, and insurance providers each have unique priorities and KPIs. Aligning them under one governance framework requires negotiation and shared accountability.
Successful IHDS models appoint joint leadership boards that oversee clinical standards, finance, and technology decisions collectively.
3. Financial and Cultural Resistance
Moving from a fee-for-service model to value-based care often meets resistance. Some providers worry that shared financial risk could reduce autonomy or revenue. Cultural resistance also appears when teams accustomed to independent workflows must collaborate within a network.
Overcoming this requires not just technology adoption, but change management programs that reframe success around patient outcomes, not patient volume.
4. Privacy, Security, and Compliance
With integration comes increased exposure to data risks. Each connected entity expands the network’s attack surface. Healthcare organizations must adopt strong encryption, role-based access control, and HIPAA/GDPR-compliant architectures to safeguard data integrity.
Beyond compliance, maintaining trust among patients and partners is crucial. A single breach can undermine confidence in the system’s ability to coordinate safely.
5. Workforce Readiness
Even with advanced digital tools, an integrated system fails if the workforce isn’t prepared to use it. Clinicians and staff need training on shared EHR platforms, communication workflows, and analytics dashboards.
The most effective IHDS implementations invest in digital literacy and provide real-time support to minimize frustration during the transition.
From Integration to Intelligence
Integration is not the endpoint — it’s the foundation for a more intelligent, adaptive healthcare system. Once organizations achieve data and process connectivity, they can unlock higher-order benefits through AI, predictive analytics, and automation.
Here’s how the next stage is taking shape:
1. Predictive Care Pathways
AI models trained on integrated datasets can identify high-risk patients before complications occur. For instance, a patient’s EHR combined with wearable data can flag early signs of heart failure, prompting timely intervention.
Predictive care transforms integration from a reactive system to a proactive one, improving outcomes and reducing hospitalizations.
2. Population Health Management
Integration gives healthcare leaders access to longitudinal data across populations. By analyzing this data, they can uncover patterns in chronic disease trends, resource utilization, or preventive care gaps.
This supports public health initiatives and enables value-based healthcare, where success is measured by improved community outcomes rather than service volume.
Population-level insight also strengthens policy design and reimbursement models — critical for government and payer partnerships.
3. Connected Intelligence Across Systems
Once hospitals, clinics, and payers share a unified data layer, analytics and AI tools can operate across the entire ecosystem. Decision-makers gain visibility into everything from referral leakage to post-discharge adherence rates.
Integrated dashboards help leadership teams evaluate performance metrics in real time, supporting agile decision-making and operational efficiency.
This kind of connected healthcare system marks the true maturity of digital transformation, where every data point serves a purpose, and every process improves with feedback.
4. Patient Empowerment Through Digital Integration
Patients are no longer passive participants. Integrated systems supported by patient portals and mobile apps give individuals direct access to records, prescriptions, and personalized recommendations.
For example, a diabetic patient can view their lab results, receive medication reminders, and schedule teleconsultations — all from one connected interface. This transparency increases engagement, adherence, and trust in the system.
How Integration Enables Value-Based Care
The healthcare industry is steadily moving toward value-based care, where reimbursement depends on the quality and effectiveness of services rather than the quantity.
Integrated systems are central to this shift because they:
- Track outcomes and performance metrics across providers.
- Reduce redundant procedures and inefficiencies.
- Align financial incentives with patient well-being.
- Support continuous improvement through analytics feedback loops.
By creating a 360-degree view of the patient journey, IHDS models make it possible to measure what truly matters — outcomes, satisfaction, and cost efficiency.
Integration and Interoperability: Two Sides of the Same Coin
Integration cannot succeed without interoperability. The latter is the technical backbone that allows different applications, devices, and databases to “speak” to one another.
An integrated system might connect hospitals and payers, but without standardized communication protocols, that connection is limited.
Your next read — Interoperability in Modern Healthcare Systems — explores how interoperability bridges technology gaps to create truly connected care networks.
The Future of Integrated Care
The future IHDS will go beyond connecting institutions — it will connect intent. Hospitals, community centers, and digital platforms will operate within shared frameworks that prioritize prevention, personalization, and participation.
Emerging trends shaping the next decade include:
- AI-driven care orchestration: Automated triage and care routing.
- FHIR-native ecosystems: Standardized data models supporting modular innovation.
- Virtual-first integration: Seamless blending of physical and digital care.
- Decentralized health data models: Patient-controlled records enhancing privacy and interoperability.
As these trends converge, healthcare will evolve from a series of interactions into a continuous, learning ecosystem.
Partnering for the Future of Integrated Care
Integration requires both technological and strategic vision. At Nalashaa, we help healthcare organizations design and implement integrated healthcare delivery systems that unify data, optimize workflows, and enable value-based outcomes.
Through our custom healthcare software development services, we build secure, interoperable platforms that support hospitals, payers, and health tech vendors across their digital transformation journey — from EHR integration to care coordination tools and analytics-driven innovation.
If your organization is exploring ways to modernize or connect its delivery systems, our team can help.
Connect with us at info@nalashaa.com to start a conversation about building technology that works as seamlessly as the care you deliver.