For healthcare payers, population health has shifted from an abstract ambition to a measurable responsibility. Outcomes influence reimbursement, quality ratings affect competitiveness, and long-term risk determines financial stability. Yet many payer organizations still rely on fragmented reporting cycles that surface insight after performance windows have already closed.
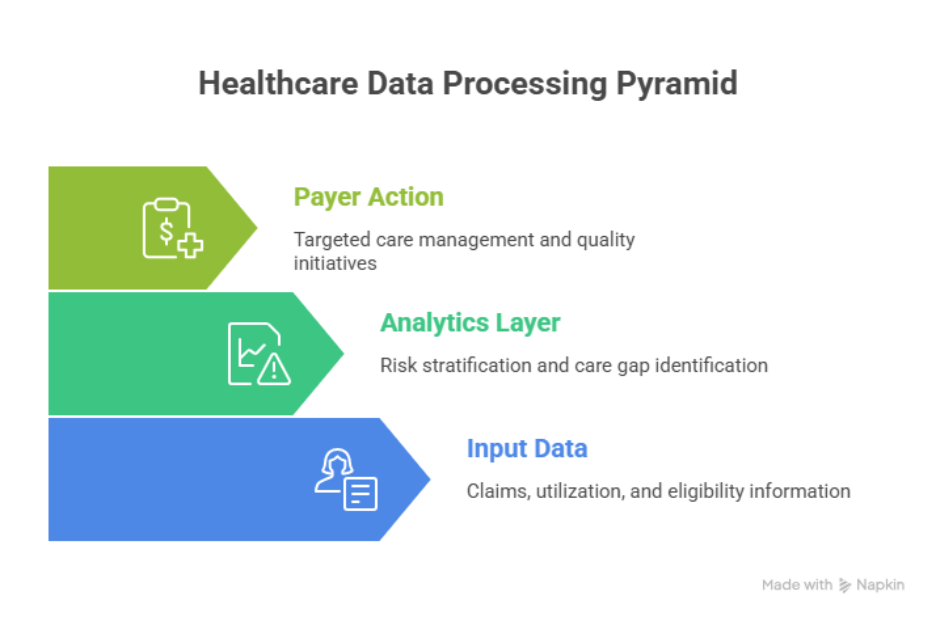
Population health analytics addresses this gap by giving payers a way to observe, measure, and influence health outcomes across entire member populations over time. Unlike provider-focused analytics, which concentrates on individual episodes of care, payer population health analytics operates at scale. It connects utilization, risk, quality, and engagement into a longitudinal view that supports earlier intervention and more informed decision-making.
This capability has become increasingly critical as value-based contracts expand and accountability extends beyond cost control into sustained outcome improvement.
Why Population Health Analytics Matters for Healthcare Payers
Payers operate across diverse populations with varying levels of risk, access, and engagement. Outcomes emerge gradually, shaped by preventive care, chronic condition management, adherence behavior, and care coordination. Traditional analytics models, built around retrospective claims review, struggle to capture this complexity.
Population health analytics enables payers to move from episodic analysis to continuous population-level insight. By integrating claims, eligibility, pharmacy, and clinical indicators, payer organizations gain a clearer understanding of how health trajectories evolve and where intervention remains possible. Essentially, population health analytics functions as one component of a broader payer analytics strategy that connects cost management, risk oversight, and outcome accountability across the organization.
For payers, this matters because:
- Financial performance increasingly depends on outcomes achieved over time
- Quality measures influence ratings, incentives, and regulatory standing
- Risk-bearing arrangements reward early identification of deterioration
- Member retention is closely tied to long-term health outcomes
Population health analytics provides the analytical foundation to manage these pressures with greater precision.
Risk Stratification for Payer Populations
Risk stratification forms the backbone of population health analytics. Payers have long classified members based on historical cost or diagnosis codes. While useful for segmentation, these static models offer limited guidance for proactive intervention.
Modern population health analytics expands risk stratification by focusing on how risk changes over time. Instead of ranking members once, payers monitor evolving risk signals that indicate potential escalation.
Key dimensions commonly included in payer risk stratification models include:
- Utilization patterns across care settings
- Chronic condition burden and progression
- Medication adherence consistency
- Preventive care completion
- Access and engagement signals
This approach allows payers to identify members whose risk trajectory is accelerating, even if the current cost remains moderate. Care management resources can then be aligned to emerging needs rather than past utilization alone.
For payer organizations, dynamic risk stratification supports:
- More effective care management prioritization
- Improved forecasting under risk-based contracts
- Earlier intervention to prevent avoidable acute events
Effective risk stratification depends heavily on the quality and consistency of claims data, which is why healthcare claims data integration remains foundational for payer analytics accuracy.
Longitudinal Outcome Tracking Across Member Populations
Outcomes rarely align with reporting cycles. Improvements in chronic disease control, preventive care uptake, or readmission reduction occur over extended periods. Snapshot-based reporting obscures this reality and limits the ability to evaluate program effectiveness.
Population health analytics enables longitudinal outcome tracking by following cohorts across time. Instead of asking whether an initiative performed well in a single quarter, payers can observe how outcomes evolve across months and years.
Longitudinal tracking supports payer organizations in several ways:
- Measuring the sustained impact of care management programs
- Evaluating outcome trends across contract periods
- Identifying populations where improvement plateaus or declines
- Aligning quality performance with financial accountability
This continuous view allows payers to refine interventions while programs remain active, rather than reacting after outcomes are finalized.
Identifying Care Gaps at Population Scale
Care gaps represent one of the most actionable applications of population health analytics for payers. Missed screenings, delayed follow-ups, and inconsistent monitoring often precede adverse outcomes and increased costs.
Population health analytics identifies care gaps by comparing delivered care against evidence-based guidelines and quality benchmarks across populations. Rather than relying on manual audits or provider-reported data alone, payers can surface gaps systematically.
Common care gap categories include:
- Preventive services not completed within recommended timeframes
- Chronic condition monitoring lapses
- Post-discharge follow-up delays
- Medication refill interruptions
Analytics allows payers to prioritize these gaps based on risk level, population impact, and likelihood of intervention success. This prioritization supports targeted outreach strategies that focus on members where closing a gap can meaningfully influence outcomes.
Turning Population Health Analytics into Daily Payer Operations
Population health analytics delivers limited value when it remains confined to dashboards or quarterly reports. For payers, its real impact appears only when insight shapes how teams work each day.
High-performing payer organizations embed population health signals directly into operational workflows. Risk indicators guide care management prioritization. Care gap insights inform outreach sequencing. Outcome trends influence how programs evolve mid-cycle rather than after evaluation periods end.
This integration requires analytics to align with decision timing. Insights surface when teams plan outreach, adjust programs, or evaluate network performance. When analytics arrive after these decisions occur, they reinforce reporting rather than control.
Operational alignment also depends on clarity of ownership. Population health analytics supports multiple functions, yet accountability for action remains explicit. Care management owns the intervention. Quality teams own their performance. Finance owns outcome-linked financial planning. Analytics serves as shared input rather than a parallel function.
How Payers Use Population Health Insight in Practice
Rather than following a single standardized model, payers apply population health analytics across several interconnected use cases.
Some teams use analytics to refine care management enrollment. Instead of broad eligibility rules, members enter programs based on evolving risk trajectories and outcome potential. This improves both efficiency and impact.
Other teams focus on program performance. Longitudinal outcome tracking highlights where engagement stalls, where improvement accelerates, and where interventions fail to influence outcomes. Programs adapt accordingly.
Network and quality teams rely on population-level insight to identify variation across provider groups. Differences in preventive care completion or chronic condition control surface opportunities for targeted collaboration rather than contract-level enforcement.
In some payer organizations, population-level utilization patterns identified through analytics also support adjacent use cases such as AI-driven fraud detection and abnormal billing pattern identification.
Across these scenarios, analytics informs direction rather than dictating action. Teams retain discretion while operating from shared, consistent signals.
Measuring What Matters in Population Health Analytics
Metrics play a central role in payer population health initiatives, yet volume often overwhelms clarity. Effective programs focus on a limited set of measures tied directly to outcomes and accountability.
Common categories include:
- Risk progression indicators, such as changes in utilization intensity or adherence patterns
- Care gap closure rates, prioritized by population risk and outcome relevance
- Outcome trend measures, tracked longitudinally rather than episodically
- Program effectiveness signals, linking intervention to measurable change
Rather than treating metrics as static scorecards, payers monitor movement over time. Improvement velocity often matters more than absolute values, especially within value-based arrangements where progress signals future performance.
Why Population Health Analytics Initiatives Stall
Despite strong intent, many payer organizations struggle to operationalize population health analytics fully. The causes rarely stem from a lack of data or analytical capability.
More often, challenges arise from misalignment.
Analytics teams generate insight without clear pathways to execution. Operational teams receive reports without confidence in definitions or assumptions. Governance frameworks remain underdeveloped, allowing multiple interpretations of the same measures.
Another common issue involves overextension. Programs attempt to address too many populations simultaneously, diluting focus and impact. Population health analytics works best when applied selectively, with clear priorities and measurable objectives.
Organizations that overcome these barriers treat analytics as an evolving capability rather than a one-time deployment. Governance, workflows, and metrics mature together over time.
Population Health Analytics in Value-Based Payer Models
Value-based arrangements amplify the importance of population health analytics for payers. Financial performance depends increasingly on outcomes achieved across defined populations rather than services delivered.
Population health analytics supports these models by providing early visibility into performance risk. Outcome trends surface before contract periods conclude. Care gaps highlight where quality measures face pressure. Risk stratification informs where targeted intervention may prevent downstream penalty or underperformance.
This visibility allows payers to adjust strategies while contracts remain active. Interventions align with outcome accountability rather than retrospective reconciliation. Provider collaboration becomes more focused, supported by shared population-level insight.
Conclusion
Population health analytics solutions have become an essential capability for healthcare payers navigating outcome accountability, cost pressure, and risk-based performance. Its value lies in the ability to observe populations over time, identify emerging risk, and act before outcomes harden into financial or regulatory consequences.
When integrated into daily operations, population health analytics enables earlier decisions, more precise resource allocation, and sustained improvement across member populations. Payers that invest in this capability position themselves to manage complexity with greater confidence and control, aligning financial performance with long-term health outcomes at scale. Connect with us at info@nalashaa.com for more information.
Latest posts by Priti Prabha (see all)
- Population Health Analytics for Healthcare Payers - January 15, 2026