For millions of Americans, filing a medical insurance claim is just the start of a long and uncertain process. In 2023, insurers on the ACA Marketplace denied 1 in 5 in-network claims, with some rejecting more than half of all submissions (Kaiser Family Foundation). The reasons behind these denials often involve missing information, manual processing errors, and slow adjudication cycles, leaving providers and policyholders frustrated.
Artificial Intelligence (AI) is helping payers combat these inefficiencies. By automating repetitive tasks, flagging inconsistencies, and identifying potential fraud in real-time, AI is transforming claims processing into a faster, more accurate, and cost-effective operation.
The Need for AI in Claims Processing
Traditional claims processing relies on manual workflows, leaving room for errors:
- High Error Rates & Claim Denials: Manual data entry, coding discrepancies, and lack of structured information can trigger claim rejections and necessitate rework.
- Slow Turnaround Times: Lengthy approvals delay provider payments, causing friction in the payer-provider relationship and potential member dissatisfaction.
- Rising Administrative Costs: Handling claims manually demands considerable human resources, significantly driving up operational expenses.
- Fraudulent Claims & Financial Losses: With vast volumes of claims to review, it becomes challenging to detect anomalies without dedicated tools.
AI addresses these issues through automated data entry, detecting errors before submission, and providing real-time fraud detection. It analyzes historical data to predict high-risk claims and highlight patterns that may otherwise go unnoticed. These advanced capabilities free up human resources for complex case evaluations and strategic initiatives
Key AI Capabilities Transforming Claims Processing
Insurance claims involve layers of verification, compliance checks, and fraud detection—tasks that traditionally slow down the process. Here’s how these technologies are making an impact.
1. Data Extraction and Validation
One of the most labor-intensive aspects of claims management is data extraction from paper or digital documents. Artificial Intelligence—particularly in the form of Natural Language Processing (NLP) and Optical Character Recognition (OCR)—enables payers to:
- Automate Data Entry: Replace manual keying with automated tools that extract patient demographics, procedure codes, and provider details from various document formats.
- Reduce Errors & Processing Time: By validating the extracted data against existing records and standardized codes, AI eliminates the need for repeated corrections.
- Improve Coding Accuracy: With NLP, AI can interpret clinical notes more reliably, ensuring that ICD-10 and CPT codes are assigned correctly.
Quicker submission of clean claims leads to fewer denials and faster adjudication.
2. Error Detection and Prevention
Errors in claims submissions can have a ripple effect, eventually increasing costs for both payers and providers. AI-driven systems excel at:
- Identifying Missing or Inconsistent Information: Claims are scanned for incomplete data or mismatched identifiers before reaching adjudication.
- Validating Coding and Eligibility: Rule-based engines, enhanced by machine learning, analyze claims against guidelines to catch upcoding, unbundling, or misfiled procedures.
- Reducing Denials: Prompt detection and preemptive correction of errors lower denial rates and minimize the rework cycle.
This layer of automated verification fosters a more predictable revenue cycle and reduces administrative back-and-forth between payers and providers.
3. Claims Adjudication Support
Claims adjudication is the backbone of payer operations, determining whether a claim is payable, partially payable, or denied based on coverage terms. AI improves this stage by:
- Providing Instant Recommendations: Machine learning models evaluate the claim against policy guidelines, suggesting approvals or flagging claims needing further review.
- Ensuring Consistency in Decision-Making: Automated checks reduce subjective biases and variations in manual evaluations.
- Speeding Up Approvals: By cutting through the manual layers, AI-driven adjudication allows payers to quickly settle straightforward claims, bolstering trust with providers.
AI transforms adjudication from a reactive, labor-intensive process into a streamlined, data-backed workflow.
4. Fraud Detection and Prevention
Healthcare fraud remains a persistent challenge, costing the industry billions every year. AI helps payers protect themselves by:
- Analyzing Large Data Sets for Irregular Patterns: Machine learning looks for anomalous billing practices, such as excessive frequency of a particular code or suspicious claim volumes.
- Real-Time Alerts: When a suspicious pattern is detected, the system can immediately flag the claim, triggering investigations or additional verifications.
- Minimizing Financial Losses: Catching fraud early avoids unnecessary reimbursements and maintains compliance with regulatory standards.
This proactive approach to fraud detection bolsters financial stability and enhances compliance within the healthcare ecosystem.
5. Predictive Analytics for Risk Mitigation
AI’s predictive capabilities allow payers to spot and mitigate risks before they escalate:
- Forecasting High-Risk Claims: Historical data and machine learning models can identify patterns in claims likely to be denied or susceptible to fraud.
- Optimizing Resource Allocation: Recognizing potential bottlenecks or areas of concern lets payers allocate staff and tech resources more effectively.
- Reducing Form Errors in Real Time: AI assists users while filling out claim forms by guiding them on what information to enter and flagging errors instantly. This reduces incorrect submissions and prevents rework.
For instance, if AI flags a claim due to a mismatch in patient history, a payer can request additional documentation immediately rather than waiting for the claim to reach an advanced denial stage.
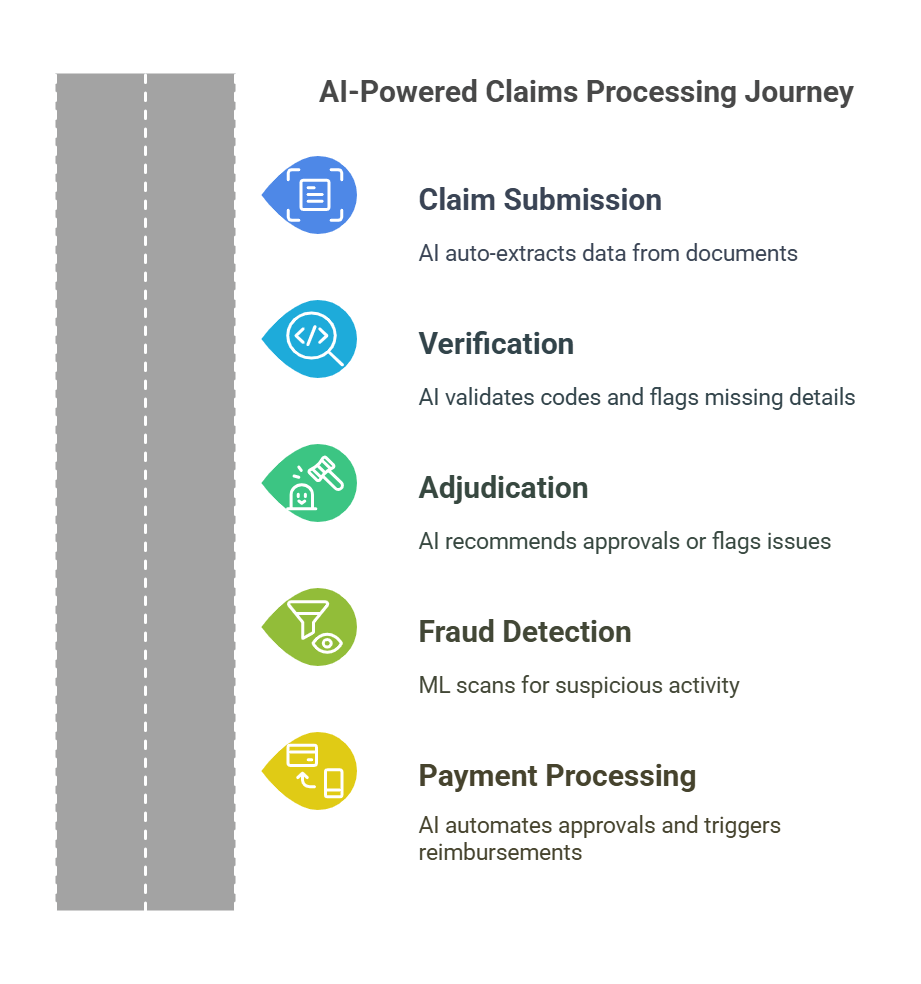
Claims Processing Journey with AI.
AI streamlines claim processing by reducing manual effort and automating decision-making at every stage. The visual below illustrates how AI enhances key steps in the claims journey, from submission to payment.
Examples of AI Technologies Used in Claims Processing
1 Natural Language Processing (NLP)
Medical documents, provider notes, and patient histories often contain unstructured text that can be difficult to process. NLP algorithms tackle this challenge by extracting relevant data—diagnoses, procedures, medications—from clinical narratives. By turning free-form text into structured insights, NLP helps:
- Improve Coding Accuracy: Automated analysis of clinical context leads to more precise coding, minimizing billing errors.
- Streamline Claims Submission: NLP tools can identify vital details like patient demographics or date of service, reducing manual input and potential oversight.
Claims submitted with accurate, comprehensive data reduce the likelihood of denials and speed up approvals, cutting administrative overhead.
2 Machine Learning Algorithms
Unlike static rule-based systems, machine learning (ML) models learn and evolve over time. By analyzing historical claims data, ML algorithms excel at:
- Detecting Fraud and Errors: They recognize unusual billing patterns, flagging high-risk claims for further scrutiny.
- Enhancing Predictive Accuracy: ML refines its predictions (for instance, about denial probabilities) as it encounters more real-world data.
- Optimizing Claims Approval: Claims with low-risk profiles can be automated for near-instant adjudication, leaving complex ones for human expertise.
Through constant iteration, ML-driven platforms become increasingly precise in identifying which claims require additional documentation or merit expedited approval.
3 Rule-Based Systems
Though AI often implies advanced machine learning, rule-based systems continue to play a crucial role in healthcare claims processing. These systems rely on predefined logic and decision trees that automatically process straightforward claims without manual intervention. For example:
- Automated Eligibility Checks: Verifying member eligibility and coverage details against policy databases.
- Policy Compliance: Matching claim details with specific payer guidelines (like maximum allowable units for a procedure).
- Quick Approval for Common Cases: Routine or standard claims can be handled in seconds, improving throughput.
Rule-based engines are especially helpful for high-volume, low-complexity claims, while more advanced AI techniques handle nuanced cases requiring adaptable analysis.
Challenges in AI-Driven Claims Processing
Despite clear benefits, implementing AI in claims operations isn’t without hurdles. Payers must address these key challenges to unlock the full potential of AI:
1 Data Quality & Standardization
AI thrives on clean, standardized data. Inconsistent record-keeping, siloed platforms, and variable data formats can impede AI’s accuracy and learning curve. Before adopting AI solutions, payers often need to:
- Consolidate Data Sources: Integrate EHRs, billing platforms, and legacy claims systems into one coherent environment.
- Establish Uniform Coding Structures: Ensure that CPT, ICD-10, and HCPCS codes align across databases.
- Implement Rigorous Data Governance: Assign data stewards and define protocols for ongoing quality checks.
Without robust data governance, even the most sophisticated AI models can struggle to deliver meaningful results.
2 Integration with Legacy Systems
Healthcare payers frequently rely on aging infrastructure that doesn’t seamlessly interface with modern AI solutions. Achieving interoperability might require significant time and capital investments. Key considerations include:
- APIs and Middleware: Building connectors between AI tools and legacy claims management software.
- System Upgrades or Migration: Weighing the cost and impact of moving from on-premise solutions to cloud-based platforms.
- Staff Training: Ensuring teams have the right skills to operate and maintain integrated systems, as well as interpret AI-generated insights.
A clear technology roadmap that factors in compliance standards and long-term scalability is critical to successful integration.
3 Need for Human Oversight
While AI excels at automating repetitive tasks and spotting statistical outliers, clinical judgment and case-by-case evaluations remain indispensable:
- Complex Cases: Claims tied to rare treatments or multiple comorbidities may require nuanced decisions beyond AI’s scope.
- Ethical and Regulatory Considerations: Certain claims might involve sensitive patient data, demanding human discretion to maintain compliance and trust.
- Continuous Model Refinement: Regular human input ensures AI models remain accurate and up-to-date, reflecting new policies or medical guidelines.
Balancing automation with expert review allows payers to harness AI’s efficiency gains while preserving patient-centric decision-making.
The Future of AI in Claims Processing
AI adoption in healthcare claims is set to deepen by advancements in automation, predictive modeling, and emerging technologies:
- Generative AI for Complex Claims: Emerging large-language models can handle intricate claim reviews or appeals, providing contextual recommendations to human adjudicators.
- Advanced Predictive Analytics: The next wave of AI solutions will proactively identify potential cost drivers, fraud hotspots, and provider performance gaps.
- AI-Driven Cost Optimization: As payers fine-tune administrative processes, they’ll use AI insights to allocate resources efficiently and offer more competitive pricing.
- Regulatory Evolution: Agencies are increasingly interested in AI’s role in healthcare, shaping guidelines on data governance, bias mitigation, and consumer protection.
Early adopters who invest in robust AI frameworks and user-friendly integrations will lead the industry in cost efficiency, error reduction, and better stakeholder experiences.
Conclusion
AI has proven its capacity to ease claims processing by faster and accurate adaptability to the growing needs of healthcare payers. Integrating technologies like NLP, machine learning, and rule-based engines, payers can streamline their operations, reduce administrative overhead, and drastically cut down on claim denials.
Although challenges such as data quality, legacy system integration, and the need for human oversight remain, these can be effectively addressed through strategic planning and phased implementation.
At Nalashaa, we help healthcare payers modernize their claims workflows with tailored automation solutions. Our expertise in AI, RPA, and intelligent data processing enables payers to streamline adjudication, minimize revenue leakage, and enhance compliance. Whether you need claims status automation, data extraction, or fraud detection capabilities, our solutions are designed to integrate seamlessly with existing systems.
Learn more about how Nalashaa supports payers or reach out to us at info@nalashaa.com to discuss your automation needs.
Latest posts by Priti Prabha (see all)
- ONC HTI 1 Final Rule and Certified APIs: A Complete Guide - February 19, 2026