Healthcare organizations handle massive amounts of data, but most of it remains unused. Less than half of structured data is actively used, and only 1% of unstructured data is ever analyzed. This disconnect has led to consequences like data breaches, outdated systems, and poorly managed records. The American Institutional Confidence poll shows that public confidence in tech companies handling sensitive healthcare data has been steadily declining. Despite these challenges, only 30% of firms have data strategies in place
Without a structured approach, data governance issues will only grow. This blog looks at what makes data governance essential in healthcare and how it can help organizations manage data better.
Challenges in Healthcare Data Governance
Effective healthcare depends on accurate, accessible, and secure data. However, managing this data comes with challenges. Data governance provides the structure and policies needed to address these challenges. Here are the issues organizations face when governance is lacking:
The Problem of Data Silos
Healthcare data is scattered across different systems like EMRs, lab databases, pharmacy systems, and insurance platforms. These systems don’t always communicate with each other, creating isolated pockets of information.
- A patient’s medical history might be available in an EMR but not reflected in the billing system.
- Lab results may be stored separately, requiring manual effort to consolidate patient records.
- Specialists in different departments often work with incomplete or outdated information.
Who Owns the Data?
In many organizations, data responsibilities are unclear. Is IT in charge? Does each department manage its own records? Who ensures data integrity?
- When ownership is undefined, inconsistencies creep in, outdated records remain in the system, duplicate entries go uncorrected, and accountability is lost.
- Without clear roles, no one takes responsibility for fixing errors or ensuring that data remains accurate and secure.
- Compliance becomes harder to enforce when there’s no designated team overseeing data usage and security.
Lack of ownership means data management often becomes reactive; problems are addressed only when they create disruptions.
Conflicting Data Sources
Multiple systems often store different versions of the same data. This creates discrepancies, making it difficult to determine which version is correct.
- A patient’s address may be updated in one system but not in another, leading to billing errors or missed follow-ups.
- Different physicians may enter diagnostic details using varied formats, causing confusion in treatment history.
- Mismatched patient records increase administrative work, forcing staff to verify details manually.
Conflicting data leads to inefficiencies and administrative burdens.
No Standard Approach to Data
Different departments use different formats, naming conventions, and data entry methods. Without standardization:
- A lab may record test results in a structured format, while a physician enters them as free text.
- Some systems store dates as MM/DD/YYYY, while others use DD/MM/YYYY, leading to misinterpretation.
- Drug dosages may be recorded in varying units, increasing the risk of prescription errors.
Without standardized data, integrating systems or running analytics becomes a challenge. Reporting inconsistencies can also make regulatory compliance complex.
Fragmented Data Accessibility
Even when data exists, accessing it isn’t always straightforward. Restrictions on data access, outdated interfaces, and lack of interoperability slow down workflows.
- Clinicians may need to log into multiple systems to retrieve a patient’s full medical history.
- Researchers struggle to extract meaningful insights when data isn’t easily retrievable or structured properly.
- Compliance teams face hurdles when conducting audits if data isn’t readily available in a standardized format
Why Data Governance Matters in Healthcare
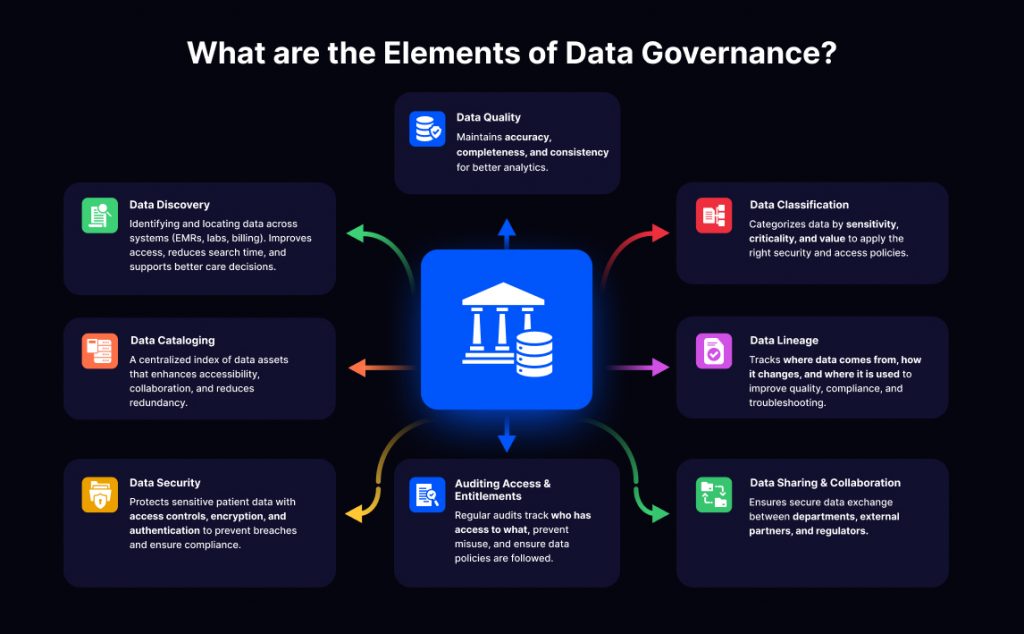
Healthcare data is only useful if it’s accurate, accessible, and secure. Without proper governance, organizations struggle with security risks, inconsistent records, and compliance issues. A structured approach ensures that data is stored and supports better decisions.
Data Security and Compliance
Healthcare organizations handle sensitive patient information that must be protected from unauthorized access, breaches, and misuse. A checklist of regulations like HIPAA, GDPR, and CCPA set strict rules, but compliance is difficult without a governance framework in place.
- Defining access rules prevents unauthorized users from retrieving or altering patient records.
- Tracking data usage through audit logs helps organizations identify security risks before they become serious problems.
- Standardizing security protocols ensures that encryption, backups, and retention policies are applied consistently across systems.
Governance provides the structure needed to meet compliance requirements while keeping patient data safe.
Improving Patient Outcomes with Better Data
Doctors, nurses, and specialists rely on medical records to make informed decisions. Poor data quality management or incomplete records can lead to errors, delays, and ineffective treatments.
- Accurate medical histories help doctors avoid misdiagnoses and prescribe the right medications.
- Complete patient records ensure specialists have the context they need when coordinating care.
- Consistent data formats make it easier to analyze patient trends and develop preventive care strategies.
With well-managed data, healthcare providers can focus on treatment rather than sorting through conflicting information.
Interoperability Across Systems
Healthcare data exists in many formats across different platforms, EMRs, lab systems, insurance databases, and more. Without governance, these systems don’t always communicate, making it difficult to get a full picture of a patient’s health.
- Standardized formats ensure that records from different sources align correctly.
- Defined data-sharing policies allow secure access between departments, hospitals, and third-party providers.
- Faster data retrieval reduces delays in care and administrative processing.
Governance creates clear rules for how data should be structured and shared, making collaboration between systems and teams easier.
Better Operations
Poor data governance slows down processes, increases administrative burdens, and creates unnecessary costs. Duplicate records, missing information, and inconsistent formats all add to the workload.
- Eliminating redundant data entry frees up time for medical staff to focus on patients.
- Reducing errors in reporting and billing prevents unnecessary disputes and delays.
- Reliable data helps management make informed decisions about staffing, budgeting, and resource allocation.
The bigger picture is that healthcare organizations already collect vast amounts of data. The real challenge is making that data accurate, secure, and accessible when it’s needed. Governance ensures that every piece of information, whether a diagnosis, a lab result, or a billing record, can be trusted and used effectively.
How to Build an Effective Healthcare Data Governance Framework
Implementing a data governance framework requires a clear plan that addresses current and future needs. Each step in the process ensures that data remains secure, accurate, and accessible. Here’s how healthcare organizations can build an effective framework:
Step 1: Identify and Categorize Data
The first step is understanding what data exists, where it’s stored, and how it’s used. This involves mapping all data sources, from patient records to operational and financial information.
- Organize by sensitivity: Separate patient health information (PHI) from operational data to ensure proper security measures are applied.
- Tag data sources: Assign labels to categorize data by type, such as clinical, administrative, or billing.
- Eliminate redundancies: Identify duplicate or outdated records to streamline storage and improve accuracy.
Clear categorization makes it easier to prioritize governance efforts and comply with regulations.
Step 2: Assign Clear Ownership Roles
Data governance requires accountability at every level. Define specific roles to ensure data quality, security, and accessibility.
- Data Owners: Responsible for the accuracy, updates, and lifecycle of specific datasets.
- Data Stewards: Handle day-to-day governance tasks, like monitoring data usage and resolving inconsistencies.
- Governance Committees: Oversee policies, enforce compliance, and coordinate across departments.
When ownership is clear, organizations avoid gaps in responsibility and ensure data is consistently managed.
Step 3: Standardize Formats and Processes
Standardization is important for eliminating discrepancies across systems and departments. Without consistent formats, data integration and analysis become difficult.
- Define templates: Create standard formats for data entry fields like dates, addresses, and test results.
- Develop uniform processes: Ensure that all departments follow the same protocols for data collection, storage, and sharing.
- Implement data validation rules: Use tools that flag errors or incomplete entries at the point of input.
Standardization minimizes errors and ensures that data from different systems align together.
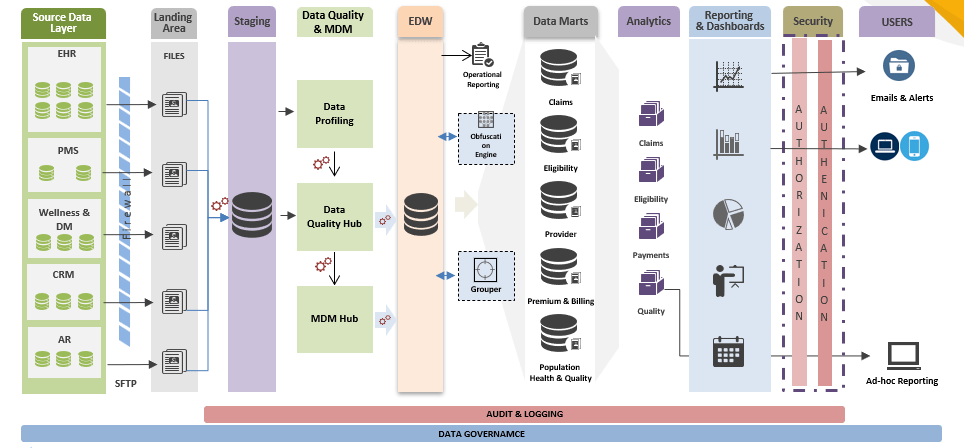
Step 4: Leverage Automation and Technology
Technology can significantly reduce the burden of manual governance tasks. Automation helps enforce policies, detect inconsistencies, and maintain compliance.
- Automate data classification: Use tools to sort and label data based on sensitivity and use case.
- Monitor access: Implement automated alerts for unauthorized access or unusual activity.
- Streamline audits: Use software to track data lineage and generate compliance reports automatically.
Step 5: Monitor and Improve Continuously
Data governance is an ongoing process that needs regular evaluation and updates. Policies that worked last year may not address emerging challenges or new regulations.
- Set performance metrics: Track key indicators like data quality, compliance rates, and user access patterns.
- Conduct regular reviews: Periodically assess whether governance policies are being followed and identify areas for improvement.
- Adapt to changes: Update frameworks to address new regulatory requirements, technology shifts, or organizational goals.
Continuous monitoring ensures that the framework evolves alongside the organization’s needs. Building an effective data governance framework takes time and effort, but the benefits are well worth it. Following these steps can turn a healthcare organization’s data into a valuable asset that supports better care.
Benefits of Data Governance in Healthcare
A well-planned data governance framework helps healthcare organizations move from managing data reactively to using it as a strategic asset. When data is reliable, secure, and accessible, providers can deliver better care, meet compliance requirements, and reduce operational risks.
Better Data, Fewer Errors
Healthcare decisions depend on accurate and complete data. When patient records are inconsistent or outdated, the risk of errors increases. Governance ensures that information stays aligned across systems, making it easier for care teams to trust the data they rely on.
- Prevents duplicate records and missing patient details.
- Reduces the time spent cross-checking data from different sources.
- Helps physicians and specialists work with the same up-to-date information.
With strong governance, data supports care rather than complicating it.
Informed Patient Care
A patient’s medical history, lab results, and treatment plans should be accessible when needed. Governance ensures that the right people have the right data—without delays or missing details.
- Physicians make treatment decisions based on complete patient records.
- Care teams avoid misdiagnoses and redundant tests caused by fragmented data.
- Patients receive more personalized care, backed by structured, reliable information.
Well-managed data doesn’t just make care more efficient—it makes it safer and more effective.
Compliance Without the Last-Minute Scramble
Data governance helps healthcare organizations meet regulatory requirements such as HIPAA, CCPA, and GDPR by establishing clear policies for data handling. Without clear governance, staying compliant becomes a constant challenge.
- Policies for data access and security reduce the risk of violations.
- Structured audit logs make compliance easier to track and prove.
- Proper data handling practices prevent breaches that could lead to penalties.
When governance is in place, compliance isn’t a box to check—it’s part of how data is managed every day.
Fewer Operational and Security Risks
Without governance, data management becomes a patchwork of manual fixes and inconsistent policies. This creates security risks and slows down operations.
- Reduces redundancies that lead to wasted time and resources.
- Prevents unauthorized access with clearly defined data permissions.
- Strengthens security by ensuring data protection measures are applied consistently.
Governance helps organizations focus on improving care and operations, rather than fixing data-related issues.
A Successful Data Governance Implementation
A well-executed data governance framework can transform how healthcare organizations manage and use data. One such example is The University of Kansas Hospital, which implemented data governance to strengthen compliance with HIPAA regulations and improve patient data management.
Eliminating the Gap Between Clinical and Operational Teams
One of the biggest hurdles was integrating data governance across different departments. Clinical teams needed data for patient care, while operational teams focused on compliance and reporting. The hospital resolved this by:
- Involving both clinical and executive leaders early in the process.
- Establishing clear governance roles to balance operational oversight with frontline needs.
- Creating policies that align data practices across departments without disrupting workflows.
This ensured that governance efforts supported both day-to-day healthcare delivery and long-term compliance goals.
Maintaining Transparency Without Compromising Security
Another challenge was making sure that users had access to the data they needed without increasing security risks. The hospital addressed this by:
- Assigning defined roles and responsibilities to data stewards and owners.
- Implementing tiered access levels to control who could view and modify patient data.
- Establishing a data audit system to monitor access and usage.
Takeaways from This Implementation
✔ Leadership Support is Essential
Data governance initiatives require executive buy-in to succeed. Senior leadership played a key role in ensuring alignment between governance policies and organizational goals.
✔ Governance is a Shared Responsibility
IT teams should not be the sole owners of data governance. Involving clinical, administrative, and compliance teams ensures that data governance policies reflect the needs of all stakeholders.
✔ More Than Just Compliance
The hospital viewed data governance not as a regulatory task, but as a way to improve decision-making, enhance patient care, and streamline operations.
How can We Help?
Implementing a robust data governance framework in healthcare is almost important in the digital age. Evaluating the ROI upfront can justify the organization’s investment and set the stage for successful implementation. Establishing a framework, defining clear roles and responsibilities, developing, and enforcing policies are the necessities of the journey.
At Nalashaa, we’ve been working with healthcare organizations for over 13 years to help them put practical data governance strategies in place. From defining roles to enforcing policies that work, we focus on custom software development solutions that fit the way your teams use data every day.
If you’re looking to improve how your organization manages its data, we’re here to help, partner with us at info@nalashaa.com.
FAQs
1. What is data governance in healthcare?
Data governance in healthcare refers to the comprehensive management of healthcare data’s availability, usability, integrity, and security. It involves implementing policies and technologies to ensure data remains accurate and secure throughout its lifecycle. It creates shared responsibilities across an organization such that all healthcare data is managed effectively.
2. What are the three pillars of data governance?
Data governance is built on three key pillars that ensure data is managed effectively:
- Data Quality – Ensures accuracy, consistency, and completeness of healthcare data across systems.
- Data Stewardship – Defines ownership and responsibility for maintaining and enforcing data policies.
- Data Protection & Compliance – Establishes security controls and ensures adherence to regulations like HIPAA and GDPR.
3. What is the role of data stewardship in governance?
Data stewards are responsible for monitoring data accuracy, enforcing policies, and ensuring data is used correctly. They act as the bridge between IT, clinical teams, and compliance officers to maintain data integrity and accessibility.
4. Who controls data governance?
Data governance is managed by a Data Governance Manager or a Chief Data Officer (CDO), depending on the organization’s structure. In some cases, the Director of Enterprise Data Management oversees governance efforts, while in others, a dedicated governance team enforces policies, ensures compliance, and coordinates between IT, clinical, and business teams to maintain data integrity and security.
5. What is the difference between data governance and data management?
Data governance defines the policies, rules, and standards for handling data, focusing on security, accuracy, compliance, and accountability. It determines who can access data, how it should be protected, and how policies should be enforced across the organization.
On the other hand, data management is the technical execution of these policies. It involves collecting, storing, processing, and distributing data so that it remains accessible, clean, and usable.
6. How does data management fit into data governance?
Data management is the technical execution of governance policies. It deals with how data is collected, processed, stored, and distributed, ensuring that data remains accessible, clean, and usable across its lifecycle.
Latest posts by Priti Prabha (see all)
- ONC HTI 1 Final Rule and Certified APIs: A Complete Guide - February 19, 2026