Electronic Data Interchange (EDI) creates a secure and common format for exchanging sensitive healthcare information between different organizations. Companies use this to communicate business documents in a standard format. It replaces paper-based documents thus saving time and minimizing errors related to manual processing. In this blog, we will explore the EDI standards for healthcare and their respective use cases.
EDI Transaction in Healthcare
EDI acts as a backbone for efficient data transmission in healthcare. Providers, payers, and clearinghouses use it to exchange business documents in a structured electronic format. It offers:
- Accuracy: Reduces errors commonly associated with manual data entry.
- Efficiency: Speeds up communication, especially for time-sensitive processes like claims and eligibility checks.
- Compliance: Adheres to HIPAA standards to maintain patient data privacy and security.
In the U.S. healthcare ecosystem, EDI solves challenges related to the vast volume of data generated daily. Medical records, insurance reimbursements, and billing information require a reliable mechanism to keep data exchange secure and error-free – and EDI fulfills this need.
EDI transactions in healthcare are standardized by the American National Standards Institute’s Accredited Standards Committee X12 (ANSI ASC X12), which defines the formats for various healthcare transactions. Any of those transactions, when performed electronically, had to adopt the specified EDI standards.
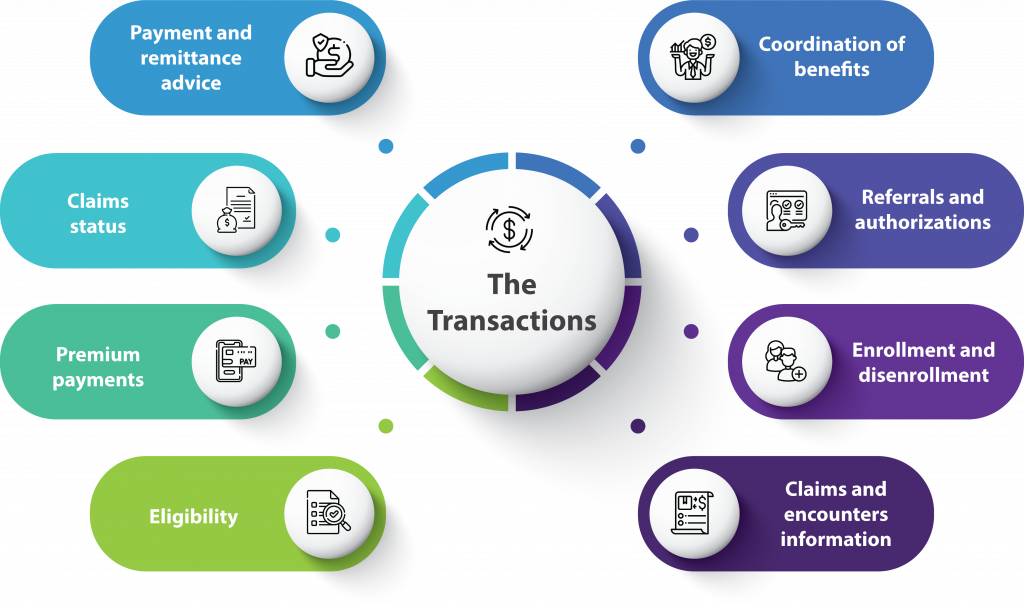
These transactions are:
EDI Standards for Healthcare and Their Use Cases
The following table summarizes key EDI standards and their applications in healthcare:
| EDI Standard | Purpose | Use Case |
| EDI 837 transaction in healthcare (Health Care Claim Transaction) | Submission of healthcare claim billing information or encounter data. | Providers send claims to payers directly or via intermediaries. |
| EDI 835 (Health Care Claim Payment/Advice) | Payment remittance advice from insurers to healthcare providers. | Insurers send payment details and Explanation of Benefits (EOB) to hospitals. |
| EDI 834 (Benefit Enrollment and Maintenance) | Enrollment of members into a payer’s healthcare benefit plan. | Employers enroll employees in health insurance plans through payers. |
| EDI 820 (Payroll Deducted Premium Payment) | Premium payment for insurance products. | Financial institutions process recurring insurance payments on behalf of providers. |
| EDI 270/271 (Eligibility Inquiry/Response) | Inquiry and response regarding healthcare benefits and subscriber eligibility. | Providers verify patient insurance coverage and benefits in real time. |
| EDI 276/277 (Claim Status Inquiry/Response) | Inquiry and response regarding the status of submitted healthcare claims. | Providers track submitted claims to monitor processing and payment timelines. |
| EDI 278 (Health Care Services Review) | Request for authorization and review of healthcare services. | Providers seek prior authorization for specific treatments or procedures. |
| EDI NCPDP (Retail Pharmacy Claim) | Submission of retail pharmacy claims to payers. | Pharmacists send prescription claim details to insurers for approval and reimbursement. |
| EDI 999 (Implementation Acknowledgment) | Confirms receipt and structural integrity of EDI transactions. | Clearinghouses confirm that submitted transactions are formatted correctly and meet required standards. |
| EDI 271/270 Addendum (Benefit Enrollment Details) | Additional inquiry and response for subscriber benefits. | Payers provide enhanced details about coverage or limitations. |
| EDI 997 (Functional Acknowledgment) | Confirmation of receipt of an EDI transaction. | Clearinghouses confirm successful receipt of healthcare transactions like claims or payment data. |
This structured approach allows organizations involved in healthcare – including providers, payers, and clearinghouses – to streamline operations and comply with regulations.
Utilize EDI to experience error-free Claims Processing.
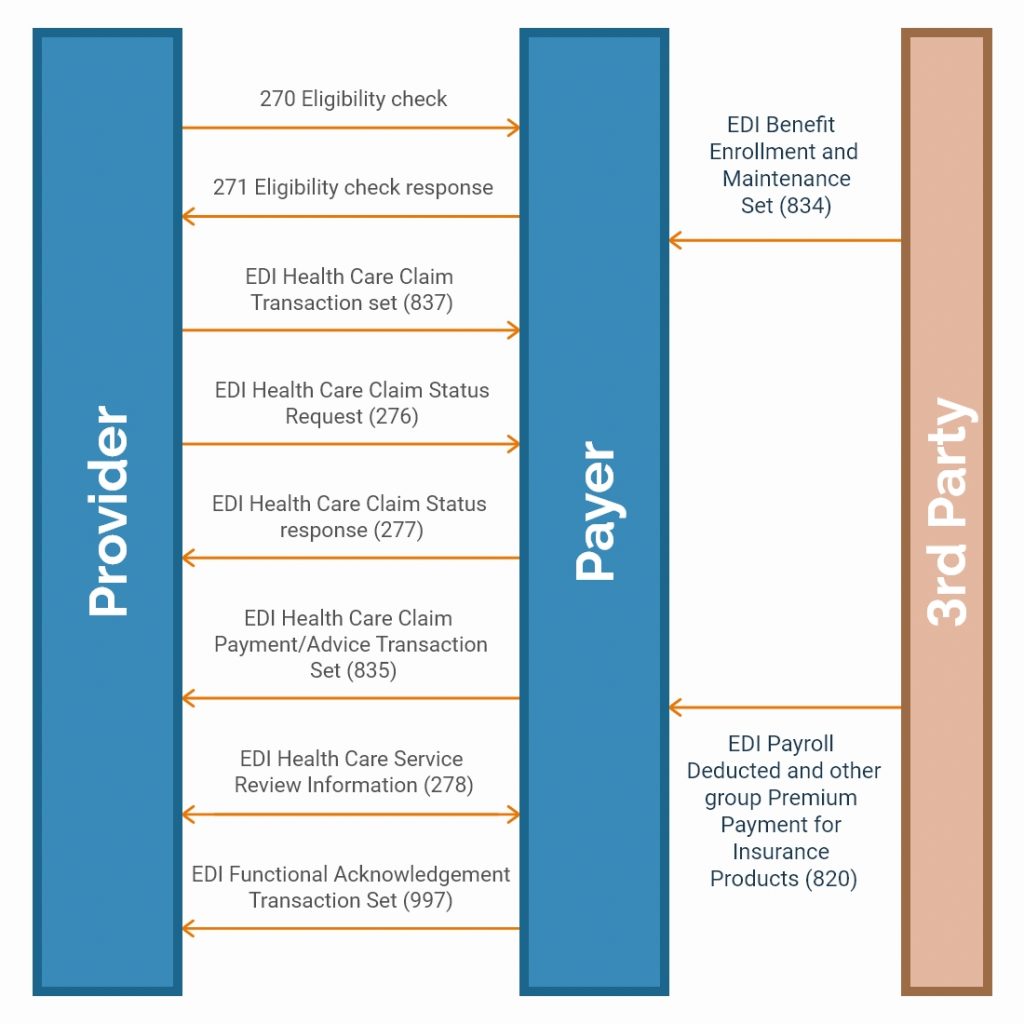
The diagram below shows the flow of EDI Standards between Providers, Payers, and Intermediaries facilitating data exchange.
Benefits of EDI in Healthcare
Healthcare organizations are benefiting from several advantages of adopting EDI. These include:
Standardization
EDI replaces fragmented and inconsistent data exchange methods with a structured, universally accepted system. Adhering to ASC X12 standards can help healthcare providers and payers exchange information without formatting issues. This eliminates misinterpretations and minimizes processing errors.
Cost Savings
EDI reduces administrative expenses by automating routine transactions. A study of the Children’s Community Health Plan (CCHP) found that digitizing data submission increased the approval rate to 99%, reducing delays and improving revenue flow. Additionally, a CAQH analysis estimates that full EDI adoption could save the healthcare industry $25 billion annually, cutting costs related to paperwork, processing fees, and labor-intensive data entry.
Data Security
EDI enhances security by using encryption protocols like Secure Sockets Layer (SSL) and Virtual Private Networks (VPNs) to safeguard patient data. Unlike paper-based transactions, where records can be lost or accessed without authorization, EDI ensures controlled access and maintains transaction logs, reducing the risk of breaches and non-compliance with HIPAA regulations.
Error Reduction
Manual entry errors, such as incorrect patient details or insurance mismatches, are a leading cause of claim rejections. Automating these transactions through EDI improves accuracy and ensures data consistency. Additionally, Snip Level validation verifies healthcare data across multiple tiers before submission, reducing denials and speeding up claims processing.
Time Efficiency
EDI reduces transaction processing times. Real-time eligibility verification allows providers to check patient coverage in seconds, avoiding service delays. According to CAQH, automating prior authorizations through EDI reduces approval times from 21 days to just a few hours, ensuring faster treatment decisions. Similarly, automated claims adjudication accelerates reimbursements, helping providers maintain steady cash flow and reducing administrative workload.
By improving coordination between payers, providers, and clearinghouses, EDI eliminates unnecessary back-and-forth communications that slow down decision-making. In emergency cases, rapid approvals for medications or procedures ensure timely patient care without bureaucratic delays.
Challenges in Implementing EDI in Healthcare
While EDI offers many benefits, organizations may face challenges during implementation:
Complex Integration Requirements: Integrating EDI with legacy healthcare systems is often challenging due to outdated infrastructure. Many systems lack compatibility with modern platforms, requiring extensive customization and testing to bridge the gaps.
High Initial Costs: The setup of EDI systems involves considerable investment in software, hardware, and training. Smaller providers may struggle to allocate the necessary budget, especially when hidden costs such as downtime and reconfiguration arise during implementation.
Compliance and Regulatory Complexity: Healthcare providers must navigate constantly changing regulations, including HIPAA updates and emerging state-level standards. Adapting to these changes often requires ongoing audits and system upgrades, demanding both time and resources.
Data Mapping and Validation Issues: Incorrect or incomplete mapping of data fields leads to rejected claims or payment delays. For example, mismatched patient identifiers or missing insurance details can cause errors that require rework and manual intervention.
Cybersecurity Risks: Despite robust encryption protocols, EDI systems remain a target for cyberattacks. Phishing attempts, ransomware, and unauthorized data access pose risks, making regular security updates and staff training on best practices essential.
Interoperability Challenges: Healthcare organizations often collaborate with multiple trading partners, each using distinct systems. Ensuring seamless data exchange across diverse platforms requires extensive coordination and rigorous testing.
Addressing these challenges requires a combination of the right technology, skilled resources, and partnerships with experienced EDI service providers to ensure smooth implementation.
How to Build an EDI-Compliant Healthcare System
Compliance with HIPAA, HITECH, and CMS regulations requires a secure infrastructure, strict access controls, and continuous monitoring to prevent data breaches and transaction failures. Organizations must structure their systems to handle sensitive healthcare transactions securely, ensuring accuracy and regulatory adherence. Below are the essential aspects of achieving EDI compliance.
1. System Architecture & Infrastructure
EDI compliance starts with a well-defined system architecture that ensures reliable data exchange and prevents disruptions.
- Scalability matters—systems must handle large transaction volumes without delays.
- Built-in redundancy prevents data loss by ensuring continuous operations during system failures.
- Automated validation mechanisms catch formatting and data-entry errors before submission, reducing rejections from payers.
- Time-sensitive transaction processing is critical—claims adjudication, eligibility verification, and remittance advice should be processed in near real-time to avoid backlogs.
2. Controlled Access & Role-Based Permissions
Access to EDI transactions should be limited based on job roles to prevent unauthorized data exposure.
- Multi-level authentication (MFA) adds an extra layer of security for users handling sensitive patient information.
- Least privilege access ensures employees only have access to the data necessary for their role, minimizing risk.
- Audit trails track all system activities, recording who accessed, modified, or transmitted data. This is essential for compliance audits and forensic investigations.
3. Encryption & Secure Data Transmission
Data security is a central pillar of EDI compliance. Encryption ensures that patient health data remains protected at every stage of transmission.
- End-to-end encryption safeguards data both in transit and at rest, preventing interception.
- HIPAA-compliant file transfer protocols such as AS2, SFTP, and MLLP must be used to securely transmit transactions.
- Digital certificates & token-based authentication help verify the authenticity of data exchanges, preventing tampering.
4. Data Integrity & Compliance Audits
To maintain compliance, organizations must implement continuous monitoring and validation mechanisms.
- Real-time transaction error detection flags missing or incorrect data before claims or eligibility checks are submitted, reducing denials.
- Automated compliance audits assess whether the system adheres to evolving EDI standards and HIPAA requirements.
- Backup & versioning protocols ensure historical records are maintained and retrievable in case of disputes or audits.
5. Incident Response & Recovery
Even with strict security measures, system failures and cyber threats remain a concern. Organizations must be prepared with a response plan:
- Rapid response protocols should be in place for handling data breaches, unauthorized access, or ransomware attacks.
- Failover mechanisms & redundant data centers allow EDI operations to continue even if primary systems are compromised.
- Regular security drills & compliance testing help detect vulnerabilities before they lead to breaches.
The healthcare industry relies on efficient and secure data exchange, and EDI addresses this need by standardizing processes and reducing errors. While challenges exist, adopting the right solutions and staying updated with technological advancements ensures success.
At Nalashaa, we bring years of experience in delivering healthcare EDI solutions for the U.S. healthcare market. Our team understands the complexities of compliance and implementation, helping organizations achieve streamlined operations. To explore how we can assist, contact us at info@nalashaa.com.
FAQs
What are the EDI standards?
EDI standards allow businesses to exchange electronic documents, automating many aspects of logistics and supply chain management. Each EDI standard comprises predefined guidelines and formats, guaranteeing consistency and interoperability between different systems and trading partners.
What is the EDI format for healthcare?
EDI (Electronic Data Interchange) X12 is a data format based on the Accredited Standards Committee (ASC) X12 standards. The Implementation Guides adopted under the Health Insurance Portability and Accountability Act (HIPAA) provide a standardized structure for transmitting healthcare transactions securely.
What are the 4 elements of EDI?
The four major components of EDI are:
- Standard document format – Defines the structure of EDI messages.
- Translation and mapping – Convert business data into EDI format and vice versa.
- Preferred communication method – Determines how EDI messages are transmitted (e.g., AS2, FTP, VAN).
- Communication network – Sends and receives documents between trading partners securely.
Who sets EDI standards?
EDI standards are maintained by various organizations. The American National Standards Institute (ANSI) chartered the Accredited Standards Committee (ASC) X12 in 1979 to develop uniform standards for inter-industry electronic exchange of business transactions.
What is EDI 211 specification?
The EDI 211 Motor Carrier Bill of Lading is a transaction set used to provide a legal bill of lading for shipments. It is utilized by shippers or other parties responsible for contracting with motor carriers and does not cover load tenders, pickup manifests, or appointment scheduling.
How many types of EDI are there?
There are over 300 different types of X12 EDI standards, each designated by a unique three-digit number. These standards cater to multiple industries, including finance, government, healthcare, insurance, and transportation.
What is the EDI standard for HIPAA?
HIPAA EDI integration standardizes the electronic exchange of healthcare information, making it easier to interpret and process across different entities. HIPAA mandates the use of ASC X12 transaction sets for electronic healthcare transactions, ensuring uniformity in data exchange.
Mitrajit Das
Latest posts by Mitrajit Das (see all)
- Revolutionizing Healthcare Communication: The AIDET Approach - March 17, 2025