Rising customer expectations have exposed the shortcomings of traditional, paper-driven claims workflows—lengthy data entry, cumbersome manual verifications, and inconsistent turnaround times. These inefficiencies strain operational budgets and frustrate policyholders and frontline staff. Automation provides a smarter alternative.
Harnessing technologies such as insurance process automation, artificial intelligence (AI), and intelligent document processing (IDP) enables claims organizations to replace time-consuming manual tasks with streamlined, error-resistant operations. In this blog, you’ll learn how automation modernizes each step of the claims process and why now is the time to make the switch.
The Burden of Traditional Claims Processing
Managing claims manually has long been a challenge for organizations, with outdated workflows leading to delays, errors, and inefficiencies. Every step—filing, submission, adjudication, and payment—relies heavily on manual intervention, creating unnecessary bottlenecks. These inefficiencies don’t just slow things down; they increase costs, impact cash flow, and lead to poor customer experiences.
Manual Complexity & Inefficiency
The claims process involves multiple steps, each requiring data collection, validation, and approval. When done manually, these steps become time-consuming and error-prone:
- Filing: Claimants fill out detailed forms, while staff manually review and enter information into systems. This increases the risk of missing or incorrect data.
- Submission: Claims are sent to different payers, each with unique formats and requirements, leading to resubmissions and further delays.
- Adjudication: Adjusters verify policy details, examine supporting documents, and check for inconsistencies—often relying on physical paperwork and multiple databases.
- Payment: Once approved, claims move through another layer of manual processing before payouts are issued, which can take weeks.
The result is long processing times, inconsistencies in claim approvals, and a lack of real-time visibility into claim status.
Impact on Stakeholders
The inefficiencies of manual claims processing affect multiple groups, each facing different challenges:
- Providers & Insurers deal with administrative burdens that slow down reimbursements and increase costs. Cash flow disruptions make financial planning difficult, while staff spend valuable time correcting errors instead of focusing on customer service.
- Patients & Policyholders struggle with unclear filing procedures and long wait times. Delayed approvals can leave them covering expenses out of pocket while waiting for reimbursement. Lack of transparency also makes it difficult to track claim status.
- The Overall System becomes more prone to fraud and inefficiencies. Manual data entry increases the risk of errors, requiring additional review and resubmissions. Fraudulent claims may go undetected due to inconsistent checks, while administrative costs continue to rise.
Traditional claims processing is expensive, slow, and difficult to scale. As claim volumes grow, these challenges only intensify, making automation a necessary shift rather than a luxury.
Why Automation Matters Now
The limitations of manual claims processing have led organizations to explore automation as a way to reduce inefficiencies and improve outcomes. A growing number of healthcare providers, insurers, and financial institutions are integrating automation into their workflows to accelerate claim settlements, minimize errors, and improve transparency.
Shifting Industry Pressures
Several factors are driving the push toward automation in claims processing:
- Rising claim volumes are making manual processing unsustainable. As the number of claims increases, organizations need scalable solutions to keep up.
- Regulatory compliance is becoming more complex, requiring detailed documentation and accurate record-keeping. Automation ensures claims adhere to industry regulations without increasing administrative workload.
- Customer expectations have shifted, with policyholders and patients expecting instant updates, faster processing times, and clear communication regarding their claims.
Leading providers and insurers are adopting automation to stay competitive, reduce costs, and meet growing industry demands. Those who continue relying on manual processes risk falling behind.
Defining Automation in Claims
Automation in claims processing is powered by several key technologies, each designed to improve efficiency and accuracy:
- Robotic Process Automation (RPA): Automates repetitive tasks such as data entry, form validation, and claims tracking, reducing the need for human intervention.
- Artificial Intelligence (AI) & Machine Learning (ML): Identifies patterns in claims data, detects fraud, and streamlines decision-making based on historical trends.
- Intelligent Document Processing (IDP): Extracts key information from scanned documents, handwritten notes, and digital records, improving accuracy and reducing processing time.
- Chatbots & Virtual Assistants: Provide real-time updates to customers, assist with claim submissions, and reduce the burden on customer service teams.
Each of these technologies contributes to a more efficient claims process, helping organizations handle higher claim volumes with greater accuracy and speed.
A Closer Look: Step-by-Step Breakdown (Manual vs. Automated)
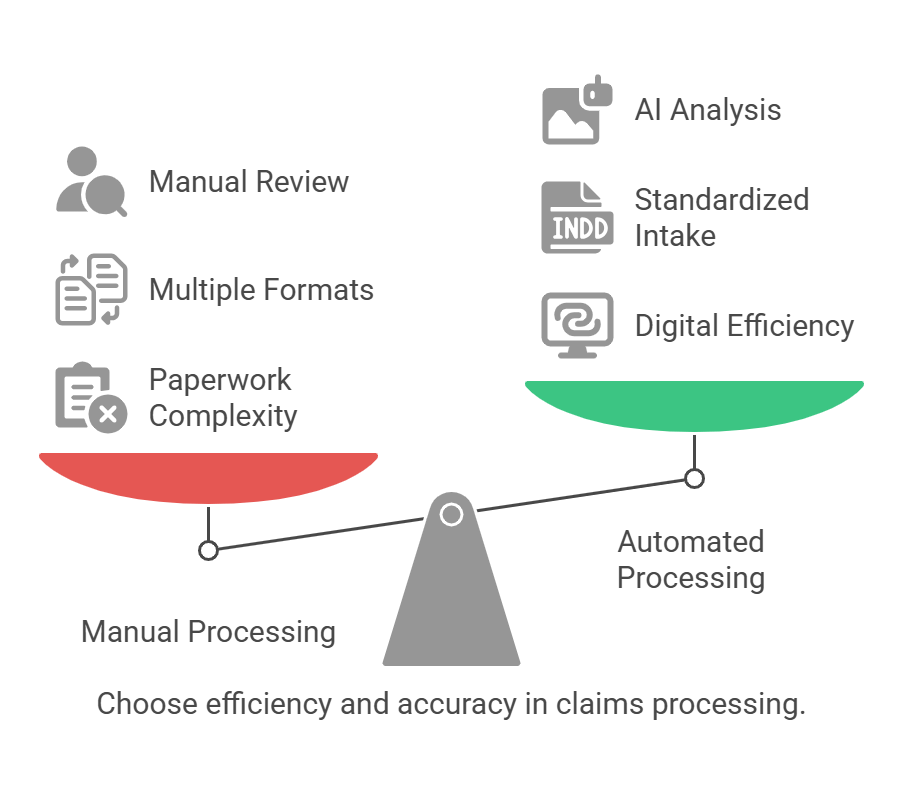
Automation transforms each stage of claims processing, replacing time-consuming manual tasks with faster, more accurate workflows. Below is a comparison of how claims are handled manually versus with automation.
Filing the Claim
- Manual: Claimants fill out lengthy paper forms, which staff must manually review and enter into the system. This process is slow and prone to missing or incorrect data.
- Automated: AI-powered forms and mobile app submissions allow claimants to enter data digitally. Intelligent systems validate entries in real time, reducing errors and speeding up the process.
Submission
- Manual: Claims must be formatted differently for various payers, often requiring rework due to missing information.
- Automated: Standardized data intake ensures claims are formatted correctly from the start. Automated validation checks flag missing or inconsistent details before submission, minimizing rejections and delays.
Adjudication
- Manual: Adjusters manually review stacks of documents, cross-checking policy details and supporting evidence. Inconsistencies lead to further delays and back-and-forth communication.
- Automated: Claims Process Automation and Machine Learning (ML) analyze claim details, highlight potential errors, and flag suspicious patterns in real time. AI-powered tools assist adjusters by providing relevant insights, reducing review time while maintaining accuracy.
Payment
- Manual: Even after approval, payments require extensive human oversight, causing delays. Repeated follow-ups are needed to ensure payouts are processed.
- Automated: Once approved, claims trigger instant payouts via digital payment systems. Real-time updates notify claimants, reducing the need for manual follow-ups.
Manual vs. Automated Claims Processing at a Glance
| Stage | Manual Processing | Automated Processing |
| Filing | Paper-based, slow, error-prone | AI-powered digital forms, real-time validation |
| Submission | Multiple formats, frequent rework | Standardized data intake, automated validation |
| Adjudication | Manual review, delays due to inconsistencies | RPA/ML-powered analysis, fraud detection |
| Payment | Human oversight, repeated follow-ups | Instant payouts, real-time updates |
By automating these processes, claims organizations can reduce delays, minimize errors, and improve efficiency across the entire workflow.
Core Automation Technologies in Claims
To achieve the benefits outlined above, claims organizations rely on a combination of automation technologies. Each plays a distinct role in streamlining claims processing and improving accuracy.
Robotic Process Automation
RPA uses software bots to handle repetitive, rule-based tasks such as:
- Data entry and validation
- Claims form processing
- Status updates and notifications
By automating these tasks, RPA speeds up claims handling while reducing human errors and administrative overhead.
Artificial Intelligence (AI) & Machine Learning (ML)
AI and ML help analyze claims data, detect anomalies, and make informed decisions. Their capabilities include:
- Fraud detection: Identifies patterns in claims data to flag potential fraud.
- Claims adjudication: Assists adjusters by predicting claim validity and providing relevant insights.
- Continuous learning: Improves accuracy over time by analyzing past claims and outcomes.
Intelligent Document Processing (IDP)
IDP extracts information from various document formats, including:
- Scanned medical records
- Insurance policy documents
- Supporting claim documentation
It converts unstructured data into usable formats, reducing the need for manual data extraction.
Optical Character Recognition (OCR)
OCR converts paper-based or image files into machine-readable text. It is particularly useful for:
- Digitizing handwritten claim forms
- Extracting key data from invoices and reports
- Making historical records searchable and accessible
Chatbots & Virtual Assistants
Chatbots help claimants with self-service options, reducing the burden on customer service teams. Key features include:
- Claim status updates: Customers can check claim progress without calling support.
- Guided claim submissions: Chatbots assist users in entering required information.
- 24/7 availability: Provides instant responses to common inquiries.
Each of these technologies plays a role in modernizing claims processing, ensuring that organizations can handle claims faster, more accurately, and with greater transparency.
Key Benefits of Claims Automation
Organizations that embrace automation in claims processing experience faster settlements, improved accuracy, and lower costs. By eliminating manual tasks and leveraging AI-driven workflows, claims move seamlessly from submission to approval. Below are some of the most significant benefits automation brings to the process.
Speed & Efficiency
Manual claims processing often results in delays due to back-and-forth communication, paperwork verification, and human intervention at every step. Automation removes these bottlenecks by accelerating repetitive tasks such as data entry, validation, and claims routing. As a result, turnaround times are significantly reduced, allowing insurers and healthcare providers to process claims faster while keeping stakeholders informed with real-time updates.
Accuracy & Reduced Errors
Data entry mistakes are among the leading causes of claim denials and rework. Automation minimizes these errors by ensuring that claim details are captured, verified, and processed with high accuracy. Intelligent systems cross-check information against predefined rules and regulatory guidelines, improving consistency in claim approvals and compliance reporting. This not only reduces administrative burdens but also ensures smoother claim resolution.
Fraud Detection & Risk Mitigation
Fraudulent claims cost insurers and healthcare organizations billions of dollars every year. Machine learning algorithms analyze patterns in claims data to detect anomalies and flag suspicious transactions before payouts are issued. By identifying inconsistencies early in the process, automation helps mitigate financial losses and enhances fraud prevention strategies, ultimately safeguarding the organization’s bottom line.
Enhanced Customer & Patient Experience
Claimants expect quick resolutions and clear communication throughout the process. Automation allows organizations to provide faster reimbursements, automated status updates, and self-service options through chatbots or online portals. A smoother experience leads to higher satisfaction levels, increasing customer trust and improving retention rates for insurers and healthcare providers.
Lower Operational Costs
Managing claims manually requires significant administrative effort, driving up costs related to labor, processing time, and error correction. Automation reduces these costs by streamlining tasks, minimizing the need for manual intervention, and allowing employees to focus on more complex cases that require human judgment. This shift not only lowers operational expenses but also improves efficiency.
Scalability & Compliance
As claim volumes grow, organizations need a system that can handle increasing demand without compromising performance. Automated workflows scale effortlessly, ensuring claims continue to be processed efficiently even during peak periods. Additionally, built-in compliance checks ensure that claims adhere to evolving regulatory requirements, reducing the risk of fines or audits. By integrating automation, organizations future-proof their claims processing operations while maintaining transparency and accuracy.
Implementation Considerations
Adopting automation in claims processing requires careful planning to ensure seamless integration and maximum effectiveness. Below are key factors organizations should consider when implementing automation.
Data Quality & Preparation
Automation tools rely on high-quality data for optimal performance. Poorly structured or incomplete data can lead to errors and inefficiencies, reducing the effectiveness of automation solutions. Ensuring that claim data is digitized, accurate, and structured properly is essential for training machine learning models and configuring automated claims rules. Organizations should invest in data validation strategies before deployment to minimize potential setbacks.
System Integration
For automation to work effectively, it must integrate seamlessly with existing claims management systems, electronic health records (EHR), and other core platforms. Compatibility is crucial—claims data should flow smoothly between systems without requiring additional manual processing. Choosing solutions with strong API and middleware capabilities helps ensure interoperability, allowing automated workflows to function without disruption.
Change Management
Automation often raises concerns about job displacement and workflow adjustments. Clear communication with employees about the role of automation—how it enhances their work rather than replacing it—is critical. Organizations should provide proper training to help staff transition to new processes and focus on higher-value tasks such as handling complex claims or improving customer interactions. A well-managed change strategy helps minimize resistance and ensures a smoother adoption of automation.
Scalability & Futureproofing
Starting small with automation, such as automating a single claims process, allows organizations to measure performance before expanding to full-scale implementation. A phased approach provides better control over deployment and enables adjustments based on real-world outcomes. Additionally, selecting a platform that can integrate emerging technologies, such as advanced AI, blockchain for claims verification, or enhanced fraud detection, ensures long-term scalability and adaptability.
Compliance & Governance
Regulatory compliance is a critical consideration in claims processing. Automated systems should include built-in compliance checks to ensure adherence to industry regulations and data privacy laws. Organizations should regularly audit automated workflows, maintain transparent decision trails for AI and machine learning tools, and ensure that automated processes align with legal and ethical standards. Implementing strong governance measures helps maintain trust and reduces the risk of regulatory violations.
Real-World Automation Use Cases
Automation has transformed claims processing for organizations facing inefficiencies, reducing delays, improving accuracy, and cutting operational costs. Below are two real-world cases where automation delivered measurable improvements.
Revolutionizing Claims Status Check with Precision Robotic Process Automation
Nalashaa worked with a prominent U.S. healthcare RCM provider to automate their claims status check process. The manual method for tracking claim statuses (Deferred, Accepted, Denied, or Closed) was time-consuming and inefficient.
Our RPA solution streamlined the process by:
- Automating claims status checks and data extraction.
- Reducing processing time by 70%, saving significant manpower.
The result? A 95% reduction in the need for manual labor and faster, more accurate claims settlements.
Know how RPA transformed claims status checks for our clients.
From Denials to Dollars: Transforming Claims Processing
A leading healthcare provider struggled with manual, error-prone data entry between their EHR system and claims forms. Nalashaa deployed intelligent data mapping to automate and streamline the process.
The solution:
- Automatically mapped EHR data to CMS-1500 and ANSI 5010 forms.
- Reduced manual effort by 85%, eliminating errors and speeding up claims processing by 70%.
This resulted in fewer claim denials, faster reimbursements, and significant cost savings.
Learn how we helped recover millions in lost revenue.
Conclusion
Claims processing inefficiencies lead to delayed reimbursements, increased administrative costs, and compliance challenges for both providers and payers. Manual workflows create bottlenecks, making it difficult to process claims accurately and on time. Automation offers a structured approach to overcoming these issues, improving speed, accuracy, and transparency in claims management.
At Nalashaa, we work with healthcare payers, insurers, and RCM companies to eliminate inefficiencies with tailored automation solutions. From claims status automation to seamless data mapping for claims processing, our expertise helps payers reduce costs, improve compliance, and enhance provider-payer collaboration.
For payers, automation strengthens claims adjudication, reduces fraud, and ensures timely payments. Our solutions integrate with existing systems, making implementation smooth while providing long-term scalability.
If your organization is looking to modernize claims processing and achieve better financial outcomes, Nalashaa is ready to help. Learn more about our payer solutions or reach out to us at info@nalashaa.com to discuss a customized automation strategy.
FAQs
1. What is healthcare claims automation?
Answer: Healthcare claims automation uses AI, machine learning, and data analytics to reduce human intervention in claims processing. It improves workflows, enhances decision-making, and streamlines tasks, leading to faster, error-free processing.
2. How does AI improve insurance claims?
Answer: AI in insurance claims helps improve claim volume forecasting by quickly analyzing claim data. Custom AI models can predict the complexity and value of claims, enabling more accurate forecasts and quicker decision-making.
3. What is the claims processing workflow in healthcare?
Answer: Claims processing in healthcare typically involves filing claims, validating data, adjudicating claims, and making payments. Automation streamlines each step, improving speed and accuracy while reducing manual errors.
4. What is Claims API?
Answer: A Claims API notifies systems about chargebacks and fraud alerts, helping improve decision-making. It allows systems to continuously learn and adapt, enhancing the claims process and improving future outcomes.
5. What is medical billing automation?
Answer: Medical billing automation uses digital tools to automate repetitive billing tasks, reducing the time spent on manual work and eliminating errors. It speeds up the billing process, ensuring accuracy and timely submissions.
6. What are the types of automation in healthcare?
Answer: The main types of automation in healthcare include fixed, programmable, and flexible automation, each with varying degrees of adaptability and use in tasks like claims processing, billing, and medical record management.
Latest posts by Priti Prabha (see all)
- ONC HTI 1 Final Rule and Certified APIs: A Complete Guide - February 19, 2026