Understanding HEDIS and NCQA
If you’re working with a health plan or on the payer tech side, you’ve probably heard HEDIS and NCQA mentioned in nearly every conversation about quality measurement. But what do they actually mean in day-to-day operations?
HEDIS, short for Healthcare Effectiveness Data and Information Set, is a set of standardized performance measures maintained by the National Committee for Quality Assurance (NCQA). These measures are used by health plans to evaluate how well they deliver care and services to members. From cancer screenings to diabetes management and mental health follow-ups, HEDIS measures cover a broad spectrum of healthcare activities that directly affect outcomes and experience.
NCQA, on the other hand, is the governing body that oversees HEDIS. It’s a non-profit organization that sets quality benchmarks for healthcare organizations. NCQA doesn’t just define metrics—it accredits health plans, sets standards for data collection, and enforces protocols that ensure consistency and reliability in reporting.
For payers, HEDIS scores influence CMS Star Ratings, member retention, and reimbursement opportunities. And because NCQA updates HEDIS annually, keeping up means adapting quickly, technologically, and operationally.
Why HEDIS and NCQA Compliance Matters for Payers
At first glance, HEDIS reporting might feel like another regulatory hoop to jump through. But for payers, it’s much more than a requirement—it’s a strategic necessity.
Why is HEDIS important?
Because it gives payers a standardized way to measure performance. Whether you’re a national insurer or a regional plan, HEDIS scores let you compare your outcomes against industry benchmarks. That’s key for identifying gaps, allocating resources, and proving value to regulators, partners, and members.
But the weight of compliance doesn’t stop at performance. NCQA standards play a major role in everything from accreditation to public rankings. Plans with strong NCQA scores are better positioned for high CMS Star Ratings, value-based contracts, and favorable placements in employer-sponsored health exchanges.
There’s also the operational side. When done right, HEDIS reporting helps:
- Pinpoint areas where care quality is slipping
- Inform care management and outreach programs
- Support population health efforts with concrete data
What makes this especially critical today is how NCQA is evolving. With a shift toward digital-first models and tighter reporting timelines, health plans that still rely on outdated tools or siloed data are going to struggle. Compliance is becoming more tech-driven, interconnected, and vital to day-to-day decision-making.
The Growing Complexity of HEDIS Compliance
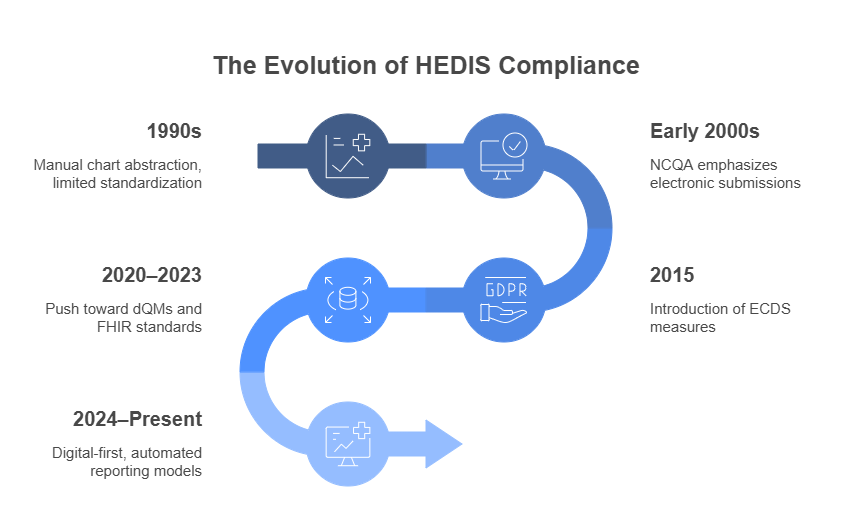
For years, HEDIS reporting operated like a checklist—review charts, gather lab results, fill in the gaps, and submit the numbers. But that model is fading fast. What we’re seeing now is a more dynamic, data-intensive approach that puts pressure on payers to modernize how they handle compliance.
One of the biggest shifts has been the move from manual chart reviews to digital quality measurement. The NCQA’s increasing focus on electronic clinical data systems (ECDS) and digital quality measures (dQMs) means health plans need to rethink how they capture, structure, and report data. Paper trails and fragmented spreadsheets simply can’t keep up.
Key Challenges for Payers:
- Data Fragmentation
Health plans often collect data from multiple sources—EHRs, labs, provider portals, pharmacy systems—but lack a unified system to bring it all together. Inconsistent formats and disconnected workflows make it hard to get a clear picture of performance.
- Manual Reporting Processes
Even with digital tools in place, many teams still rely on manual steps to compile reports. This increases the risk of errors and delays, especially when reporting cycles tighten or measure definitions change.
- Evolving NCQA Guidelines
NCQA isn’t static. Each year, it updates its HEDIS measures and reporting requirements. For payers, that means constant adaptation—not only in terms of measure logic but in how their tech systems support new data types and formats.
This growing complexity makes one thing clear: staying compliant is about whether your infrastructure is built to support the level of accuracy, speed, and interoperability that NCQA now expects.
How Smarter Tech Stacks Simplify Compliance
The complexities of HEDIS and NCQA compliance aren’t going away, but how health plans respond to them can change dramatically with the right technology stack. Payers that adopt more agile, interoperable systems are not only keeping pace with compliance updates—they’re turning reporting into a strategic function.
Data Collection and Integration
The first hurdle in compliance is always data. Getting the right data, from the right place, in the right format, on time.
- Interoperability with EHRs, Labs, and Pharmacy Systems
Health plans must pull data from a diverse mix of sources, often outside their own ecosystem. Platforms that support real-time data exchange using standards like FHIR make it easier to sync with provider systems, labs, and other third-party sources. This reduces lag and increases data accuracy.
- Unified Data Views Through Aggregation
Aggregation engines consolidate clinical and claims data into a centralized view. This not only simplifies analysis but ensures that all relevant inputs for HEDIS measures are captured without duplication or omission.
- From Manual to Digital Quality Measures
Traditional chart-chasing is being replaced by digital quality measures derived from ECDS. These measures pull data directly from electronic sources, streamlining input and enabling real-time tracking. Instead of periodic snapshots, payers gain continuous visibility into performance across their member populations.
Automation in Reporting and Analytics
Once the data is in place, the next step is to turn it into something useful and fast. That’s where automation moves from convenience to necessity.
- Auto-Generated HEDIS Reports
Modern reporting tools can generate HEDIS submissions automatically based on configured logic. This cuts down the manual lift for compliance teams, reduces the chance of human error, and helps meet NCQA deadlines without the last-minute scramble.
- Dashboards for Tracking and Audit Readiness
Visual compliance dashboards offer measure-by-measure real-time insights into where a plan stands. These tools help teams identify reporting gaps, monitor and measure trends, and flag risks before an audit reveals them.
- Data-Driven Decision Making
Integrated analytics platforms let payers go beyond scorekeeping. They help uncover patterns across member groups, providers, and conditions. That means you’re meeting benchmarks and using the data to improve outcomes, design smarter outreach, and support population health goals.
The key here is speed and precision. Automation doesn’t replace compliance teams—it gives them the bandwidth and tools to focus on the work that drives quality, not just reporting.
Enablers of Smart Compliance
Behind every high-functioning compliance process is a stack of technologies designed not just for scale, but for adaptability. As HEDIS and NCQA evolve, so should the tools used to meet their standards.
- FHIR (Fast Healthcare Interoperability Resources)
FHIR is the foundation for modern data exchange in healthcare. Built to streamline the sharing of clinical information, FHIR enables standardized communication between payers, providers, labs, and other health IT systems. For NCQA-aligned digital quality measures, FHIR-native systems drastically reduce integration headaches.
- Open Health Stack (OHS)
Developed as part of the digital public infrastructure movement, OHS includes open-source tools built specifically for FHIR-based apps. Payers adopting OHS components can quickly spin up digital tools for tracking, validating, and analyzing quality data—all while staying aligned with NCQA’s future direction.
- Cloud-Based Platforms
Cloud infrastructure brings flexibility and version control that’s critical when NCQA updates reporting logic or new measures are introduced. Cloud-native solutions support real-time updates, easier scaling, and lower IT overhead—freeing payer organizations to focus on reporting accuracy, not system maintenance.
Is Your Payer Tech Stack Compliance-Ready?
Checklist Items:
- ☐ Supports FHIR-based data exchange
- ☐ Integrates with multiple data sources
- ☐ Automates HEDIS report generation
- ☐ Supports ECDS and digital measures
- ☐ Real-time analytics and dashboards
- ☐ NCQA audit trail features built-in
Preparing for the Future of HEDIS
The future of HEDIS is already taking shape—and it’s digital, data-driven, and fast-moving. NCQA isn’t just nudging health plans toward modernization; it’s fundamentally rethinking how quality is measured and reported. For payers, staying ahead means aligning their technology roadmap with NCQA’s evolving vision.
- Digital-First Measurement Models
NCQA is steadily phasing out reliance on manual abstraction in favor of digital quality measures (dQMs). These are calculated using structured data from EHRs, health information exchanges, and other interoperable sources. The goal is to make reporting more continuous, less disruptive, and far more reflective of real-time care quality.
- FHIR-Based ECDS (Electronic Clinical Data Systems)
FHIR is now central to how data will be transmitted and validated. NCQA is embracing FHIR-based ECDS as a standard pathway for capturing and submitting clinical quality data. This shift supports automation, reduces administrative overhead, and enables a level of interoperability that legacy systems simply can’t match.
- Allowable Adjustments for Population-Specific Measures
Recognizing the diversity of health plan populations, NCQA is introducing allowable adjustments—customizations that retain the clinical intent of measures while accommodating local realities. But using these adjustments effectively requires data infrastructure that can filter, segment, and apply logic dynamically across populations.
What This Means for Payers
Smarter tech stacks aren’t just about meeting compliance requirements—they’re about creating a framework that’s ready for what’s next. Whether it’s adapting to new measure specifications or integrating with national data hubs, payers with modern, FHIR-aligned systems will move faster and with less friction.
Building a Compliance-Ready Infrastructure
HEDIS and NCQA compliance today demands more than accurate reporting—it requires infrastructure that can keep up with the pace of regulatory change, the complexity of digital data, and the pressure to prove value.
For payers, the shift isn’t just about meeting requirements. It’s about building a system that reduces manual lift, adapts quickly to NCQA updates, and delivers insights that improve outcomes. A modern tech stack makes that possible. It brings interoperability to the forefront, streamlines digital quality measurement, and turns fragmented data into a strategic asset.
The payoff? Faster audits, fewer errors, and a clearer view of how well care is delivered across every population segment.
Need to modernize your HEDIS and NCQA compliance approach?
Nalashaa helps payers build smart, scalable systems for continuous readiness—combining interoperability expertise, automated reporting, and cloud-native architecture to support every stage of the compliance lifecycle with healthcare payer technology solutions.