In healthcare, time spent on documentation often translates to time taken away from patients. Physicians juggle between diagnosing, prescribing, and entering notes into electronic systems — a process that remains one of the most significant pain points in clinical workflows. Manual data entry not only slows down appointments but also leads to fatigue and inconsistencies in record-keeping.
AI is changing that narrative. The advent of AI-powered speech-to-text and generative technologies is reshaping how clinicians capture, structure, and submit patient notes. Instead of typing or dictating into rigid templates, providers can now speak naturally, with AI transcribing, formatting, and structuring information in real time. The result? Documentation completed up to 2x faster, higher accuracy in patient records, and significantly reduced provider burnout.
This transformation is now taking shape through virtual assistant–based documentation systems, which bring intelligent, voice-driven workflows directly into clinical environments.
Defining AI in Clinical Documentation
AI in clinical documentation extends far beyond speech recognition. It integrates machine learning, natural language processing, and generative AI to understand medical context, identify relevant clinical entities, and structure unorganized voice inputs into readable, compliant, and actionable notes.
With this intelligence embedded, clinical documentation becomes an adaptive, context-aware process. Instead of manually entering details, healthcare providers can simply speak — and the system automatically:
· Transcribes speech to text with medical-grade accuracy (up to 95–98%), ensuring high fidelity even with diverse accents and clinical terminologies. This minimizes the need for manual edits, reducing post-transcription correction time by nearly 60%.
· Applies AI-driven templating to structure content as SOAP (Subjective, Objective, Assessment, and Plan) or consultation notes, standardizing documentation formats automatically. This reduces note creation time by 40–50%, while ensuring consistency across providers and specialties.
· Learns clinician preferences over time, adapting to their documentation style, frequently used terms, and tone. Over sustained usage, this personalization boosts transcription accuracy by 15–20%, making AI-generated notes almost indistinguishable from manually curated ones.
· Integrates directly with existing EHR systems for seamless submission, eliminating manual copy-paste or uploads. This streamlines record updates, enabling clinicians to finalize and store notes 30% faster, while maintaining full compliance and traceability.

Where AI Accelerates the Workflow
The influence of AI becomes most visible across the stages of a clinician’s note-taking and submission lifecycle. The design of such intelligent documentation tools focuses on making each step faster, more intuitive, and less error-prone.
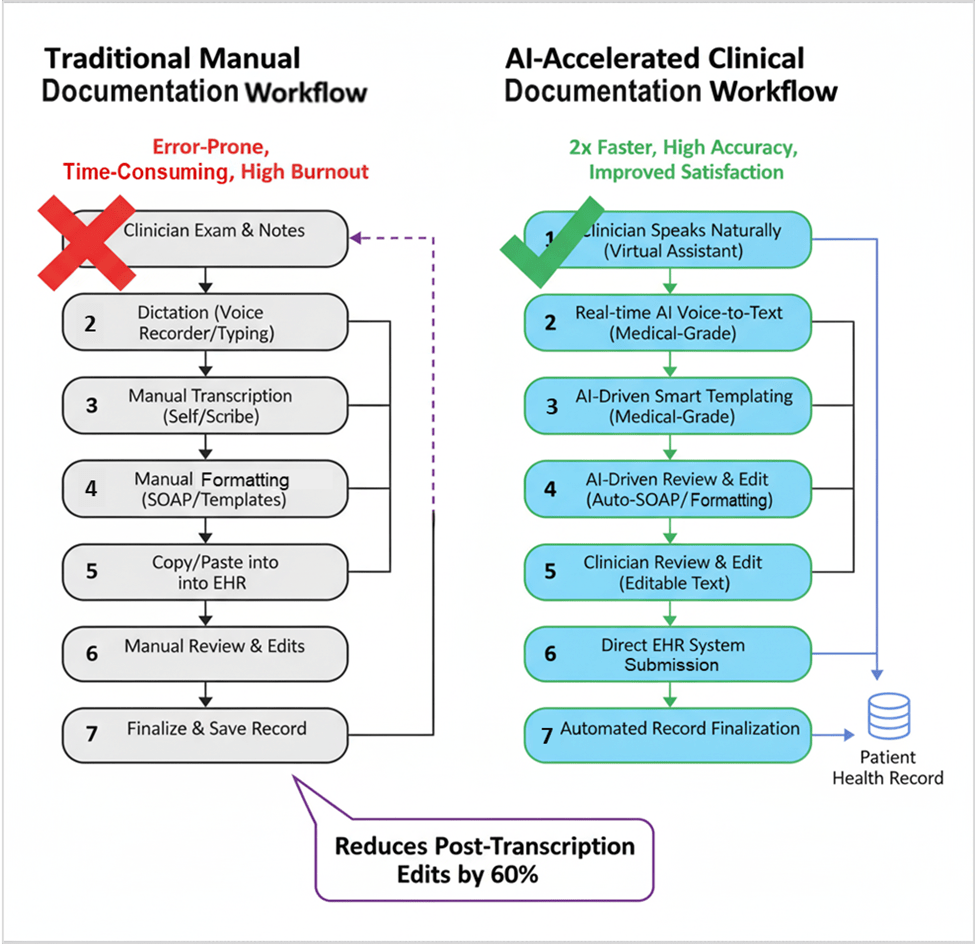
1. Voice-to-Text Transcription
With a single click, clinicians activate real-time voice capture, powered by advanced speech-to-text engines. The transcription appears instantly on screen, supported by intuitive controls to pause, resume, clear, or save. AI ensures high-quality transcription even amid conversational speech, reducing manual corrections by nearly 60%.
2. AI-Driven Note Structuring
Once transcription is saved, OpenAI-powered text generation transforms unstructured notes into standardized templates — such as consultation or progress notes.
This automation eliminates repetitive formatting, enabling providers to move from free speech to structured clinical notes in seconds.
3. Review and Submission
Clinicians can review, edit, or enhance AI-generated notes within an editable text area. Once satisfied, they submit directly into their system of record, with built-in confirmation prompts ensuring data integrity. A final screen confirms successful submission, completing the workflow without any context switching.
4. Mobile-Responsive and Seamless Experience
Built with a fully responsive frontend, modern AI documentation systems ensure that physicians can document care on desktops, tablets, or mobile devices — providing flexibility across practice settings.
Together, these features reduce note creation time by over 50%, enhance documentation accuracy, and enable clinicians to focus more on patient interaction than on data entry.
From Speed to ROI: The Payoff of AI in Clinical Workflows
The impact of AI in documentation extends beyond faster typing or transcription. It translates directly into operational efficiency and financial return.
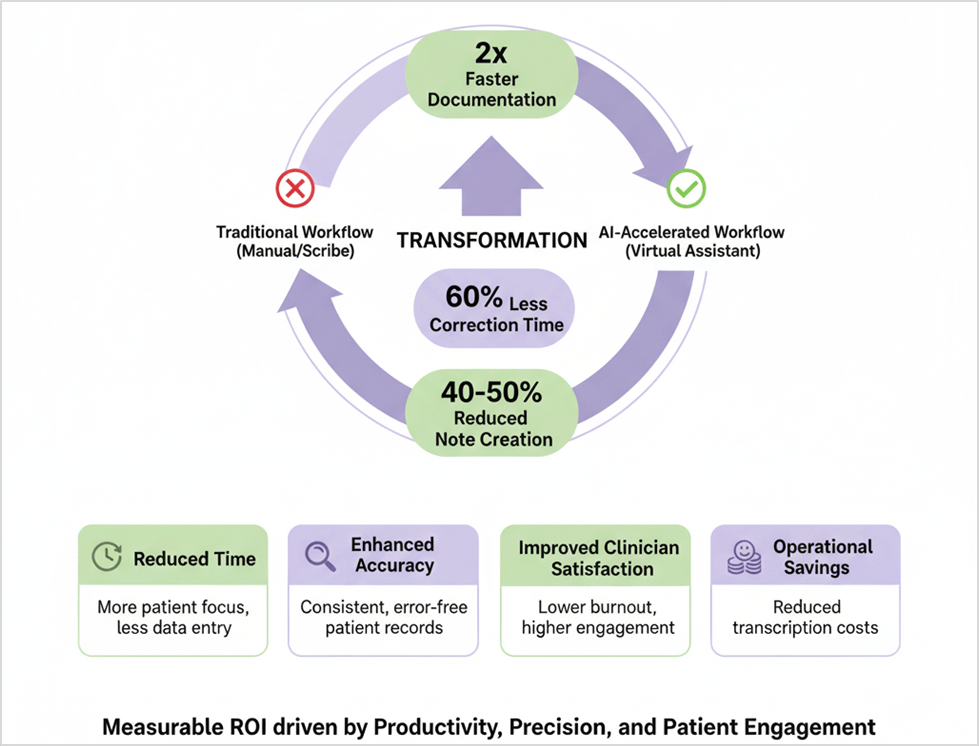
· Reduced documentation time: Physicians complete notes up to 2x faster, freeing time for additional patient consultations or value-based tasks.
· Enhanced accuracy: AI minimizes transcription errors and ensures consistency in structured notes, reducing rework cycles.
· Improved clinician satisfaction: By offloading repetitive note-taking, providers experience lower cognitive load and higher engagement.
· Operational savings: Healthcare organizations reduce costs associated with transcription services and post-visit record corrections.
For healthcare providers, this means a measurable ROI driven by productivity, precision, and improved patient engagement — the core pillars of digital transformation in modern healthcare.
Making AI-Driven Documentation a Reality
Implementing AI in healthcare documentation requires thoughtful integration, not disruption. Successful implementations show how to layer intelligence over existing workflows rather than replacing them.
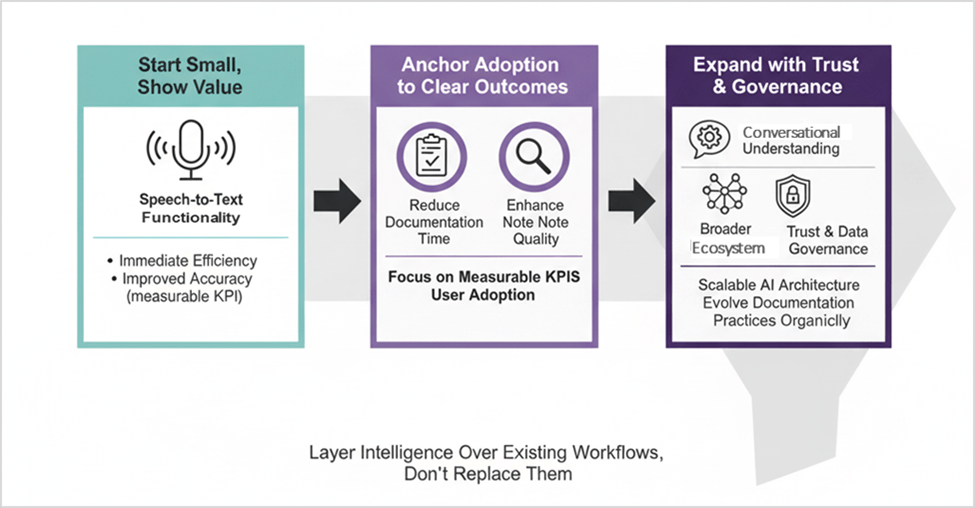
Start small, show value: Begin with speech-to-text functionality to demonstrate immediate improvement in clinician efficiency and accuracy.
Anchor adoption to clear outcomes: Focus on reducing documentation time and enhancing note quality — both measurable KPIs that accelerate user adoption.
Expand with trust and governance: Once the foundation is in place, extend capabilities toward conversational understanding, context-based responses, and broader ecosystem integration.
By combining user-centered design with scalable AI architecture, healthcare organizations can evolve documentation practices organically, ensuring both adoption and sustainability.
Building Healthcare Software with Intelligence at the Core
Traditional EHR systems have long struggled to balance usability and compliance. AI changes that equation. With intelligence embedded into the documentation process, healthcare applications redefine how providers interact with technology — not as a barrier but as a partner in care delivery.
When healthcare documentation becomes conversational, it frees providers to focus on empathy, insight, and clinical excellence. What starts as an AI-assisted transcription tool evolves into a smart virtual assistant, capable of understanding context, suggesting responses, and learning continuously from usage patterns.
The next era of healthcare will belong to organizations that weave AI into their operational DNA. Intelligent documentation is an early step in that journey — a proof point that automation doesn’t just save time, it redefines value in patient care.
For organizations exploring intelligent healthcare solutions, now is the time to act. To learn more about building AI-driven healthcare experiences, connect with us at info@nalashaa.com.