Cybersecurity alerts. Data silos. Staff retyping information between systems. These are not edge cases; they are daily realities in U.S. hospitals. Research shows that nearly three-quarters of healthcare providers continue to run legacy systems, from outdated EHR modules to imaging platforms and billing applications. These tools still function, but they create risks every time data needs to move between them.
Instead of attempting costly replacements, many organizations are choosing healthcare legacy modernization through integration. Using healthcare automation tools, legacy EHR integration, and FHIR-based connectors, hospitals can link older platforms with newer applications to improve compliance and streamline operations. In this article, we will look at what counts as a legacy system in healthcare, the risks they carry, and how integration is shaping a safer and more connected future.
What is a Legacy System in Healthcare?
A legacy system in healthcare is best recognized by its constraints. These are applications or platforms that still support essential workflows but fall short on modern demands like real-time interoperability, scalability, and secure data handling.
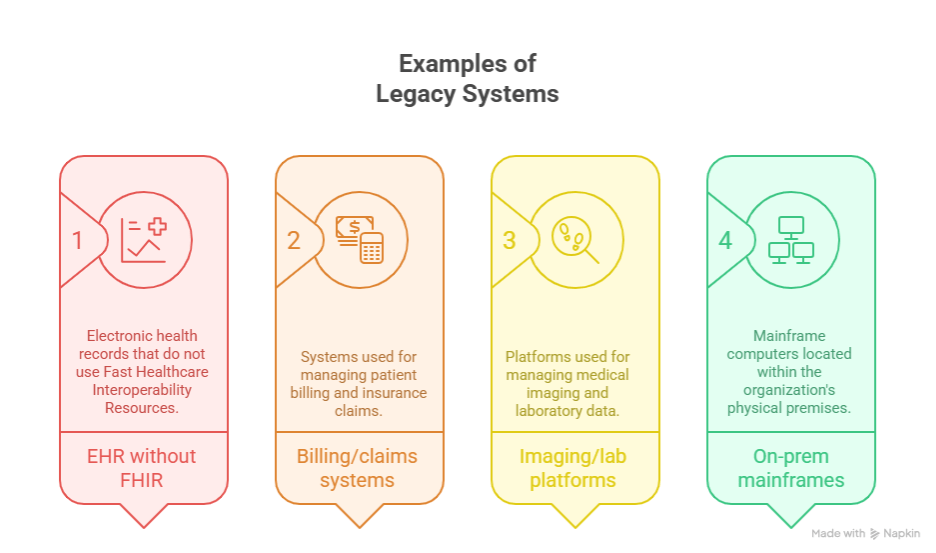
They exist in many forms:
- Electronic Health Records (EHRs) without FHIR support, forcing custom workarounds to connect with new applications.
- Billing and claims platforms built on outdated file structures that resist automation.
- Imaging and lab systems locked into proprietary formats that delay information sharing.
- On-premise mainframes still running scheduling or claims processing across large hospital networks.
The distinction comes down to adaptability. A modern platform integrates seamlessly with other systems and keeps pace with regulatory standards. A legacy system lags behind, creating silos and extra work for staff.
Many of these platforms remain central to care delivery and financial operations, but their limitations turn them into obstacles for organizations pursuing healthcare legacy modernization. Recognizing them early helps leaders decide when to apply legacy EHR integration, when to use healthcare automation tools, and when a full replacement is the wiser option.
Hidden Costs of Legacy Systems
Legacy systems rarely collapse overnight. Instead, they create a steady drain on budgets, security, and staff productivity that builds up year after year.
Compliance exposure
Older platforms struggle to keep pace with evolving standards. Some cannot support modern audit trails, while others are unable to meet interoperability mandates like the ONC’s information blocking rule. Each gap forces hospitals into custom fixes that add complexity and delay compliance.
Cybersecurity vulnerability
Unsupported operating systems and outdated applications make healthcare networks easier targets. Breaches are increasingly costly, and every unpatched module or outdated database widens the attack surface. For leadership, the real issue is not whether an attack will happen, but how large the damage will be if legacy systems remain exposed.
Operational inefficiency
Legacy systems increase staff workload in subtle but expensive ways. For example, a billing platform may require files to be exported as CSVs before uploading to a payer portal. These kinds of workarounds slow down processes, frustrate employees, and introduce unnecessary errors. Over time, they become a hidden source of waste and burnout.
Integration complexity
Connecting old systems with new tools often takes more effort than expected. Legacy platforms may use proprietary data formats or undocumented customizations. Integration projects frequently run over schedule because mapping fields, testing connections, and validating workflows are more complicated than they first appear.
Maintenance overhead
Keeping legacy systems alive requires niche expertise and ongoing infrastructure support. Hospitals sometimes maintain redundant servers or keep outdated operating systems running simply for compatibility. This maintenance tax locks budgets into survival mode and diverts resources away from innovation.
The cumulative effect is clear: even when they appear stable, legacy systems undermine compliance, security, and performance. Leaders evaluating modernization must weigh these hidden costs alongside the investment required for integration or replacement.
Why Integration Beats Replacement
Healthcare leaders often assume the only options are to continue with outdated systems or to replace them entirely. Integration provides a third path that preserves existing functionality while adding modern capabilities.
Maintain daily operations with less disruption
Replacing an EHR or billing platform is disruptive, often requiring months of retraining, reconfiguration, and testing. Integration allows hospitals to maintain continuity while gradually plugging in new tools. For instance, FHIR-based connectors can make data accessible to modern applications without tearing out the entire backend.
Balance cost and return
Full system replacements demand large upfront investments, which many hospitals cannot sustain. Integration allows spending to be spread across phases, with each project delivering tangible value. This phased approach makes modernization more manageable and allows organizations to adjust as priorities shift. Hospitals that reach a tipping point often look toward cloud migration for healthcare systems as the next stage in their modernization roadmap.
Preserve institutional knowledge and customization
Over the decades, hospitals have built specialized workflows and reports within their legacy systems. Full replacement risks losing these customizations or forcing disruptive changes on staff. Integration protects that institutional knowledge while enabling a gradual transition to modern platforms.
Reduce risk to patient care
Shutting down a legacy platform entirely can cause downtime or gaps in access to patient information. Integration lowers this risk by keeping core systems active while adding layers of functionality. This ensures continuity of care while modernization takes place in the background.
Support future scalability
Healthcare needs are expanding rapidly with telehealth, remote monitoring, and AI-driven analytics. Legacy systems alone cannot keep up, but integration makes it possible to extend capabilities step by step. Hospitals can adopt new tools as needs arise without committing to a complete overhaul.
Integration is not a shortcut but a strategic option that balances cost, continuity, and future growth. For many organizations, it is the only viable way to modernize while protecting ongoing patient care.
Integration Approaches for Legacy Systems
Legacy integration in healthcare is not one-size-fits-all. The right method depends on how old the system is, what kind of data it holds, and how modernization goals are prioritized. Most organizations end up using a combination of approaches to minimize disruption and maximize value.
API gateways and system wrappers
When a legacy application cannot connect directly with modern platforms, developers often create a wrapper or gateway. This serves as a translator, converting legacy data into formats that newer systems can process. For example, a billing or scheduling system can be exposed through an API layer without altering its core code.
HL7 and FHIR bridges
Clinical data standards are central to interoperability. Older EHRs often work only with HL7 v2, while newer platforms expect FHIR. Integration engines can bridge these standards, allowing lab results, medication records, and care plans to flow securely between systems. This method brings older platforms into alignment with current interoperability requirements without replacing them.
Robotic process automation as a connector
Some systems are too rigid for APIs or middleware. In those cases, robotic process automation can act as a bridge. RPA bots simulate human keystrokes and clicks, transferring data from one system to another. This is particularly useful for processes such as claims entry or eligibility checks, where interfaces are limited, and it connects directly with how AI in revenue cycle management, from denial prediction to cost saving, is reshaping financial workflows.
Data migration versus real-time integration
Hospitals face a choice between migrating data or leaving it in place. Migration is effective for historical information that needs to be archived in a central repository. Real-time integration is essential when legacy platforms remain in use but must continuously share data with modern systems. Choosing the right balance ensures compliance and avoids duplicating effort.
Middleware and integration engines
When multiple systems need to exchange information, middleware provides a hub. Integration engines handle transformation, routing, and security, so each system only connects once. This approach reduces complexity and gives hospitals a scalable foundation for future projects.
These approaches give organizations flexibility. They can choose methods that fit their current environment while building toward long-term modernization goals.
Key Benefits of Legacy Integration in Healthcare
Integration delivers more than technical connectivity. It shapes how hospitals function and how smoothly staff can care for patients.
Improved interoperability
With integration in place, clinical and administrative data flows across systems. A lab result entered in one application can be available to a physician in another without manual uploads. This reduces silos and gives clinicians faster access to complete patient information.
Stronger compliance and security
Routing data through standardized interfaces allows hospitals to enforce encryption, audit logging, and access controls even when the legacy platform lacks these features. This creates a compliance layer that keeps organizations aligned with regulations while extending the useful life of older systems.
Reduced manual effort
Workarounds like exporting CSV files or retyping data between applications vanish once integration is established. Automated data flows free staff from repetitive tasks, which reduces administrative waste and improves morale.
Extended lifespan of core platforms
Replacing a legacy system outright is often delayed because of cost and disruption. Integration allows hospitals to continue using these systems while enhancing them with modern capabilities. This stretches their value and buys time for thoughtful, phased modernization.
Readiness for new technology
Modern initiatives such as AI-driven analytics, remote monitoring, and patient portals depend on connected data. Legacy integration makes that data available, ensuring hospitals can adopt new tools without waiting for a full system replacement.
For leadership, these benefits highlight that integration is not just an IT project. It is a strategy to balance stability with innovation.
Challenges of Legacy Integration
Integration comes with its own hurdles. Hospitals that underestimate them risk creating fragile solutions instead of sustainable modernization.
Governance and oversight
Connecting disparate systems raises questions of data ownership and accountability. Without clear governance, integration may create conflicting records or inconsistencies that are harder to resolve later.
Vendor lock-in
Legacy platforms often use proprietary data structures. Some vendors limit database access or charge heavily for integration support. This restricts flexibility and requires strong negotiation to avoid long-term dependency.
Complexity of mapping workflows
Many legacy applications have been customized over decades. A field repurposed for billing or reporting in one hospital may not serve the same function elsewhere. Transferring such fields without careful mapping risks inaccurate or corrupted data.
Change management
Integration alters the way staff interact with systems. Even small changes can disrupt long-standing habits. Without planning and training, adoption will lag, and staff may revert to manual workarounds that undermine the project.
Balancing short-term fixes with long-term goals
Quick connectors solve immediate needs but create technical debt if deployed without a strategy. Hospitals must weigh urgency against sustainability, ensuring integrations are built with the future in mind.
These challenges emphasize that integration is not a shortcut. Success requires governance, vendor alignment, and a roadmap that ties each project to broader goals for healthcare legacy modernization.
Conclusion
Legacy systems remain the backbone of many hospitals, but their limitations create risks and inefficiencies that grow harder to ignore. Replacing them outright is often unrealistic, which is why integration has become the practical path forward. By using approaches such as API wrappers, HL7/FHIR bridges, and selective automation, providers can modernize step by step while keeping critical operations running.
At Nalashaa, we help organizations design the right integration strategy for their needs. Our healthcare automation solutions support legacy EHR integration, interoperability projects, and modernization roadmaps that reduce risk while unlocking new possibilities.
Ready to see how integration can extend the life of your systems and prepare your organization for the future? Let’s start with a conversation about your current workflows and data challenges. Contact us at info@nalashaa.com.
Latest posts by Priti Prabha (see all)
- ONC HTI 1 Final Rule and Certified APIs: A Complete Guide - February 19, 2026