Prior authorization is intended to control costs and ensure medically necessary care, but the reality is not ideal. The manual process is slow, expensive, and inefficient, contributing to care delays, administrative burdens, and high denial rates. 90% of physicians report that prior authorization has negatively impacted patient outcomes, and 80% have seen patients abandon treatment due to delays (AMA).
With rising compliance mandates, staffing shortages, and the demand for real-time healthcare, automating prior authorization has become necessary. This article explores the challenges of manual PA, the benefits of automation, and how health plans can successfully transition to an automated system.
The High Cost of Manual Prior Authorization
Prior authorization is meant to ensure that medically necessary and cost-effective treatments are approved. However, the way it’s currently managed often works against its purpose. Instead of streamlining care, the manual process adds layers of complexity, slowing down approvals, overburdening staff, and leaving patients frustrated.
For health plans, the inefficiencies of manual prior authorization translate into significant financial losses, compliance risks, and poor provider and member experience.
- Time-Consuming and Resource-Intensive
Every prior authorization request involves multiple stakeholders, paperwork, and back-and-forth communication between providers and payers. This process, when done manually, is incredibly slow:
- Each request takes an average of two full workdays to process.
- Physicians spend over 14 hours per week dealing with prior authorizations instead of treating patients.
- 87% of prior authorizations are still processed via fax, phone calls, and portals that require manual data entry, leading to errors and missing documentation.
For patients, these delays can mean the difference between timely treatment and worsening health conditions.
- Rising Administrative Costs
Processing prior authorizations manually doesn’t just cost time, it costs money. With each request requiring human intervention, staffing expenses skyrocket:
- Health plans spend over $18.4 billion annually on processing prior authorization requests.
- Each manual request costs between $80 and $130, adding a financial burden to both payers and providers.
- The need for specialized staff, such as nurses, call center executives, and prior authorization specialists, further increases operational costs.
Compliance Risks & Regulatory Pressures
Beyond financial costs, non-compliance with prior authorization regulations puts health plans at risk of fines and legal complications. The Centers for Medicare & Medicaid Services (CMS) is enforcing stricter rules, requiring:
- Urgent requests are to be processed within 72 hours and standard requests within seven days.
- Clear explanations for denials, ensuring transparency for providers and members.
- Public reporting of prior authorization performance metrics, holding health plans accountable.
With these new regulations set to take effect in January 2026, health plans that fail to modernize risk facing penalties, reputational damage, and provider dissatisfaction.
Provider Burnout and Member Frustration
A poorly managed prior authorization process directly affects the people who rely on them.
- 92% of care delays are linked to administrative inefficiencies in prior authorization.
- 80% of physicians say manual prior authorizations have led to patients abandoning treatment.
- Many payers outsource prior authorization handling to third-party vendors, adding another layer of complexity that further frustrates both providers and members.
When authorizations are denied or delayed without clear explanations, members feel ignored and mistreated, leading to a decline in trust in their health plan. Providers, meanwhile, spend valuable hours fighting denials instead of delivering care.
How Automation Transforms Prior Authorization
Manual prior authorization is a slow process with too much paperwork, and delays. Automation changes this completely. Instead of getting caught up in back-and-forth paperwork, AI and digital workflows can handle most of the process instantly. Let’s break down what a fully automated prior authorization process looks like compared to the outdated, manual approach.
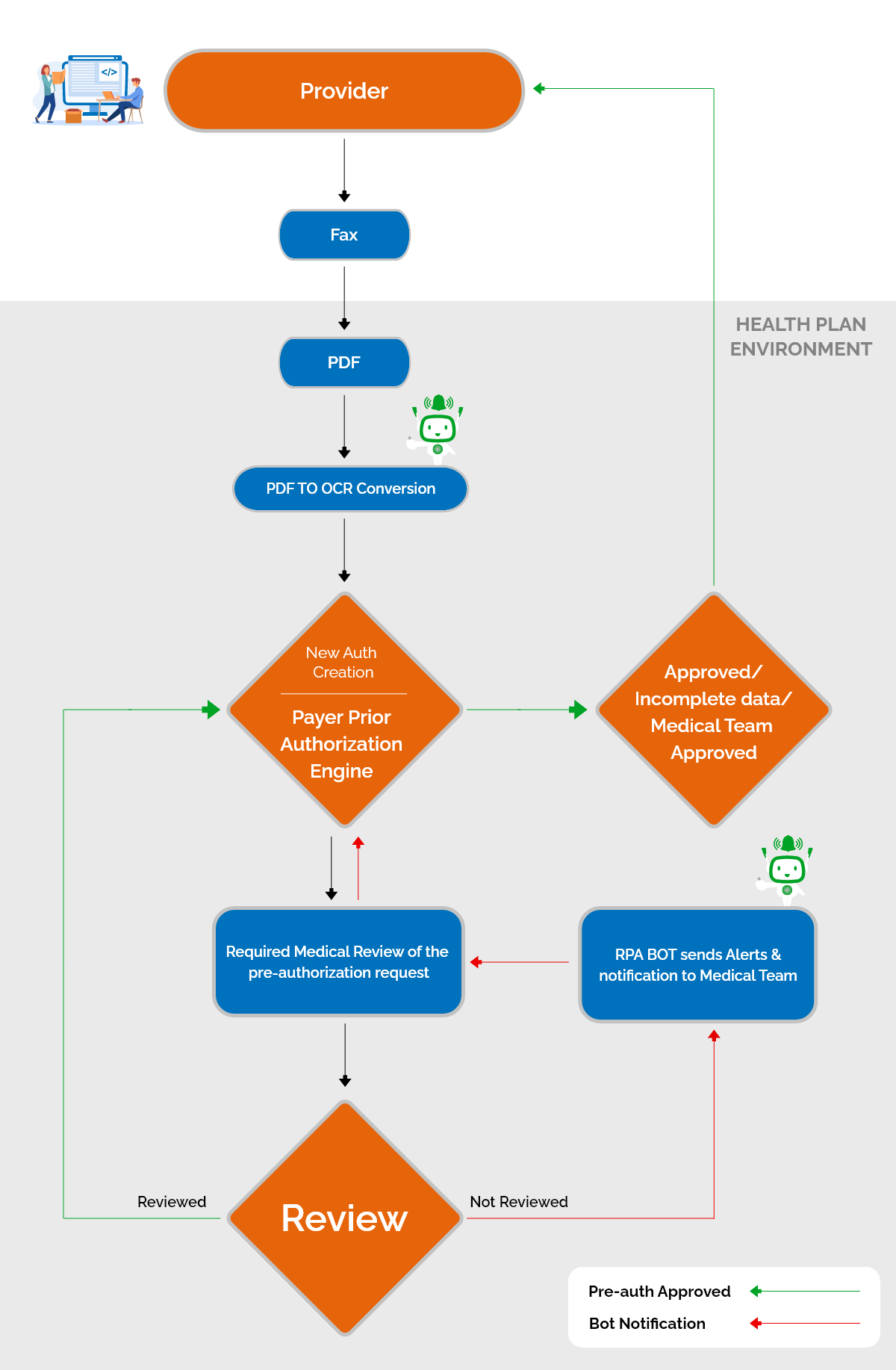
Here’s a Pictorial Representation example of RPA Bots’ work for a Pre-Authorization Request from the Provider
Faster Approvals, Fewer Delays
Manual prior authorization is slow because every request goes through multiple touchpoints, often getting stuck in fax queues, phone calls, or incomplete submissions. A single request can take days or even weeks before it’s approved.
Automation removes these roadblocks.
- Routine approvals happen instantly because AI systems can verify requests against payer policies in real time.
- No more unnecessary back-and-forth if documents are missing, the system flags them immediately instead of providers finding out days later.
- Urgent cases get priority, ensuring that life-saving treatments aren’t held up by administrative red tape.
A doctor ordering an MRI shouldn’t have to wait five days just to hear back from an insurance company. With an automated system, that approval happens in minutes, not days. Patients get faster treatment, providers aren’t left waiting, and payers reduce processing workloads.
Slashing Administrative Costs
Processing prior authorizations manually is expensive. Health plans spend millions each year just to keep up with paperwork, staffing, and call center operations.
- Each manual request costs between $80 and $130 in administrative expenses.
- Annual spending on prior authorization processing is over $18.4 billion—a cost that keeps rising as the number of requests grows.
- Staffing shortages make things worse, leaving existing teams overwhelmed and increasing the risk of errors.
Automation cuts these costs drastically. Instead of spending resources on manual paperwork, AI-driven bots handle document verification, eligibility checks, and approvals, reducing the need for large administrative teams. Payers can redirect savings into improving member benefits instead of maintaining outdated systems.
Compliance Without the Hassle
Regulations around prior authorization are getting stricter, and health plans that don’t adapt will struggle to keep up.
- By 2026, CMS mandates require urgent requests to be processed within 72 hours (or seven days for standard requests).
- Payers must provide clear explanations for denied requests—no more vague rejections.
- Health plans will have to publicly report their prior authorization performance, meaning inefficiencies won’t go unnoticed.
With automation, compliance becomes easier.
- AI-powered tracking ensures every request is processed on time, avoiding penalties.
- Automated denial explanations ensure providers and members understand why a request was rejected.
- Real-time status updates keep everyone informed, reducing provider frustration and appeals.
Instead of struggling to meet regulatory deadlines, automated systems ensure compliance from day one.
A Better Experience for Providers and Members
For providers, manual prior authorization is one of the most frustrating parts of patient care. They waste time on phone calls, faxes, and portal logins when they should be treating patients. For members, it’s equally frustrating—not knowing if their treatment will be covered, waiting too long for approvals, and dealing with unexpected denials.
- 92% of care delays are linked to manual prior authorization inefficiencies.
- Many payers outsource prior authorization handling to third-party vendors, which only adds more confusion and delays.
Automation simplifies the process for everyone involved.
- Providers can submit and track requests directly through their EHRs, eliminating unnecessary steps.
- Members get real-time updates, so they aren’t left in the dark about their approvals.
- AI-powered queue management ensures urgent cases are prioritized, so no patient is left waiting longer than necessary.
Instead of being a frustrating bottleneck, prior authorization becomes a seamless, transparent process that helps members get care faster and with fewer headaches.
The Technologies That Enable Prior Authorization Automation
Automating prior authorization is about building a system that works faster, smarter, and with fewer errors. That’s where AI, interoperability, and robotic process automation (RPA) come in.
With the right technology, health plans can streamline approvals, reduce costs, and stay compliant without extra effort. Let’s look at the technologies that make this possible.
AI-Powered Decision Support
AI can evaluate requests instantly, identifying which ones can be approved automatically.
- Routine requests can be auto-approved based on payer policies, cutting wait times from days to minutes.
- AI identifies missing documentation before submission, preventing unnecessary denials.
- Machine learning models recognize patterns in previous approvals and denials, improving decision accuracy over time.
For example, if a provider submits a request for a commonly approved diagnostic test, AI can immediately cross-check it against the member’s plan and approve it without human intervention. This means faster treatments and fewer appeals.
Interoperability & Real-Time Data Exchange
One of the biggest reasons prior authorization is so slow is the lack of seamless data sharing between providers and payers. Right now, many approvals require faxing documents, making phone calls, or re-entering information into multiple systems.
Automation solves this through interoperability, allowing different systems to talk to each other in real time.
- FHIR (Fast Healthcare Interoperability Resources) APIs enable direct data exchange between EHRs and payer systems.
- Prior authorization requests can be submitted and approved directly from a provider’s EHR, reducing the need for duplicate data entry.
- Automated status updates ensure providers and members always know where their request stands, eliminating status inquiry calls.
For example, instead of a provider calling a payer to check approval status, the EHR can pull live updates directly from the payer’s system, keeping everyone informed instantly.
3. Robotic Process Automation (RPA) for Repetitive Tasks
A lot of prior authorization work is repetitive data entry, document matching, and status tracking. This is where robotic process automation (RPA) comes in.
- RPA bots handle administrative tasks, like checking for missing information and verifying eligibility.
- They can automatically pull required documents, reducing manual effort for providers.
- Status updates and notifications are triggered instantly, keeping workflows moving smoothly.
Automated Queue Management & Prioritization
Not all prior authorization requests are equal. A routine medication refill request shouldn’t get stuck in the same queue as a life-saving surgery approval.
Automation helps by prioritizing requests based on urgency.
- High-priority requests (like emergency procedures) are automatically moved to the front of the queue.
- Non-urgent requests are processed in the background, ensuring everything moves efficiently.
- AI-driven risk scoring identifies cases that may need additional review, reducing unnecessary delays.
Transparent & Automated Denial Management
One of the biggest frustrations in prior authorization is unclear denials. Providers often don’t know why a request was rejected, leading to endless appeals and resubmissions.
Automation solves this with structured denial explanations and proactive issue detection:
- AI generates clear denial explanations, helping providers understand exactly what’s missing or incorrect.
- Predictive analytics detect patterns in denials, helping payers and providers prevent repeat mistakes.
- Automated appeals submission allows for faster reconsideration, reducing the back-and-forth delays.
Turning Challenges into Opportunities
For years, prior authorization has been seen as a necessary burden, a system that ensures cost control but often at the expense of efficiency. The shift toward automation is about creating a smarter, more responsive healthcare system where payers, providers, and patients all benefit.
Health plans that modernize their approach now will have a significant advantage. With regulatory deadlines approaching and provider expectations rising, those who continue relying on fragmented, manual workflows will struggle to keep up. The transition to AI-driven, interoperable systems is becoming the industry standard.
How Nalashaa Solutions Can Help
At Nalashaa Solutions, we specialize in helping health plans eliminate the complexities of prior authorization with intelligent healthcare automation solutions. We don’t offer off-the-shelf solutions—we build tailored automation frameworks that fit seamlessly into your existing systems.
Instead of reworking legacy processes, we help you reinvent them, so your operations aren’t just faster, but also more transparent and provider-friendly. Let’s talk about how we can streamline your prior authorization process. Connect with us at info@nalashaa.com to explore a solution that works for you.
Latest posts by Priti Prabha (see all)
- Inside the Surescripts Network: How eRx Gets Delivered Safely - June 10, 2025