Healthcare delivery has always revolved around one challenge: how to bring the right care to the right person at the right time. But as populations age, chronic illnesses increase, and healthcare costs rise, traditional systems have struggled to keep up. Today, new models of care and technology-driven innovation are redefining how services are organized, delivered, and experienced.
Understanding the types of healthcare delivery systems is essential for anyone shaping the future of healthcare. Each type has a specific purpose, structure, and technology footprint, and together they form a network that supports modern, connected, patient-centered care.
What Are Healthcare Delivery Systems?
A healthcare delivery system is the framework through which care is provided, financed, and coordinated. It includes hospitals, clinics, community programs, home-based services, and digital platforms that work together to maintain health, treat illness, and improve outcomes.
Every system aims to balance four goals:
- Accessibility: Ensuring patients can reach the care they need.
- Quality: Delivering evidence-based, consistent treatment.
- Continuity: Sharing information seamlessly across providers.
- Efficiency: Using resources wisely to reduce waste and cost.
While each country’s system looks different, most delivery models can be grouped into a few broad categories that reflect how care flows from prevention to recovery.
Types of Healthcare Delivery Systems
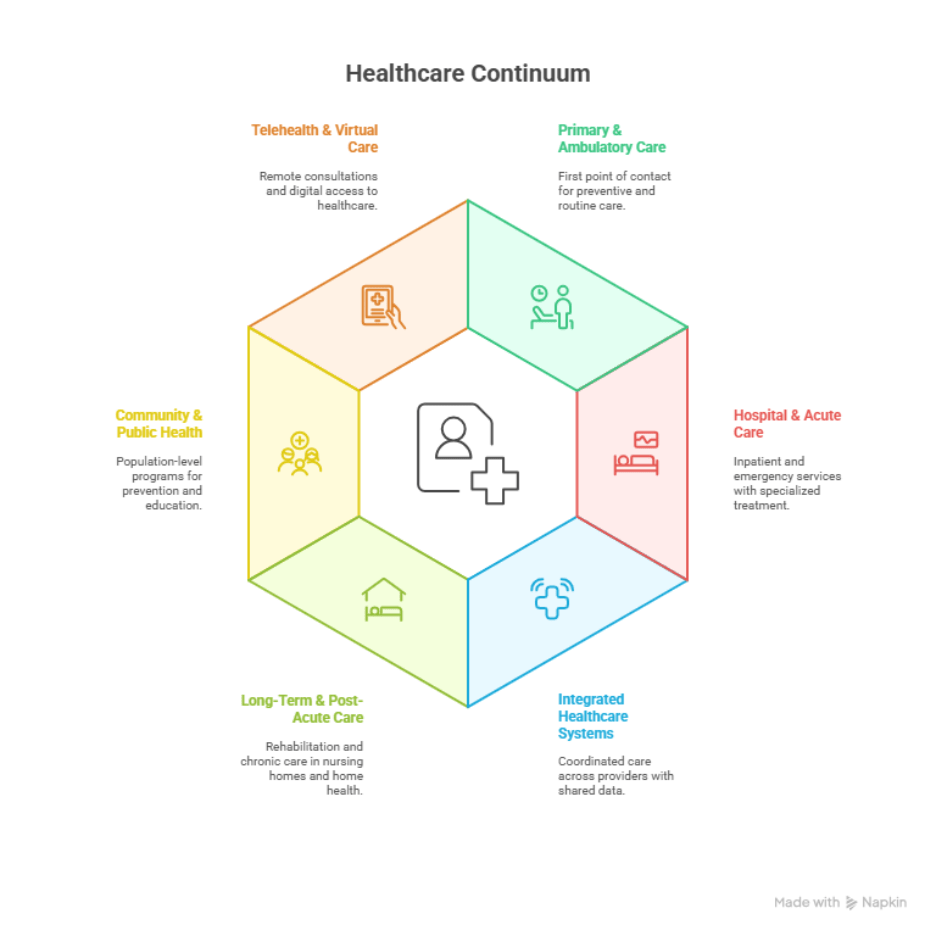
1. Primary and Ambulatory Care Systems
Primary care is the foundation of all healthcare delivery systems. It provides first-contact, continuous, and comprehensive care through physicians, nurse practitioners, and community health centers.
These systems emphasize preventive services such as screenings, immunizations, and chronic disease management. Increasingly, primary care is supported by digital scheduling, online portals, and teleconsultations, allowing clinicians to manage more patients efficiently and stay connected between visits.
Challenge: Maintaining coordination with specialists and hospitals while managing growing patient loads.
2. Hospital and Acute Care Systems
Hospital systems handle complex and emergency cases that require advanced equipment, specialized staff, and intensive monitoring. They represent the secondary and tertiary layers of healthcare delivery.
These systems are evolving from static institutions to dynamic, data-driven environments. Predictive analytics, connected monitoring devices, and electronic record systems are helping hospitals anticipate patient needs, allocate resources more efficiently, and reduce medical errors.
Challenge: Balancing cost, capacity, and post-discharge continuity of care.
3. Integrated Healthcare Delivery Systems
An integrated healthcare delivery system unites hospitals, clinics, physicians, laboratories, and payers under a coordinated network. Instead of treating each facility as a silo, it connects them through shared governance, financing, and information systems.
When a patient moves from primary care to a specialist or from hospital to rehabilitation, their data follows automatically. This integration reduces duplicate tests, prevents medication errors, and ensures consistent treatment.
Example features: Shared electronic health records, population health analytics, and unified care teams.
Challenge: Achieving interoperability and cultural alignment across multiple organizations.
4. Long-Term and Post-Acute Care Systems
These systems support patients who need extended care, rehabilitation, or daily assistance due to chronic illness, injury, or age. They include nursing homes, rehabilitation centers, hospice programs, and home-based services.
Technology now plays a central role in these environments. Remote monitoring devices track vital signs in real time; digital dashboards help caregivers manage visits, and secure messaging keeps families informed.
Result: Greater independence for patients and fewer hospital readmissions.
Challenge: Workforce shortages and the cost of implementing connected tools at scale.
5. Community-Based and Public Health Systems
Community health systems focus on prevention and population health. They deliver services like immunization drives, maternal care, nutrition programs, and disease surveillance.
Technology enables these systems to gather real-time data, track health indicators, and deploy targeted interventions. For example, digital registries and mobile health platforms help monitor outbreaks or measure the success of vaccination campaigns.
Challenge: Funding limitations and inconsistent infrastructure between regions.
According to the World Health Organization (WHO), community-based care is essential for improving equity and achieving universal health coverage.
6. Telehealth and Virtual Care Systems
Telehealth has become a standalone layer within modern healthcare delivery systems. Through video consultations, mobile health apps, and wearable sensors, patients can connect with providers without visiting a facility.
For rural populations, telehealth technology bridges geographic gaps. For specialists, it enables follow-up care and collaboration with primary providers. Virtual wards and remote patient monitoring systems have turned homes into extensions of the hospital network.
Result: Lower costs, faster intervention, and more continuous engagement between patients and clinicians.
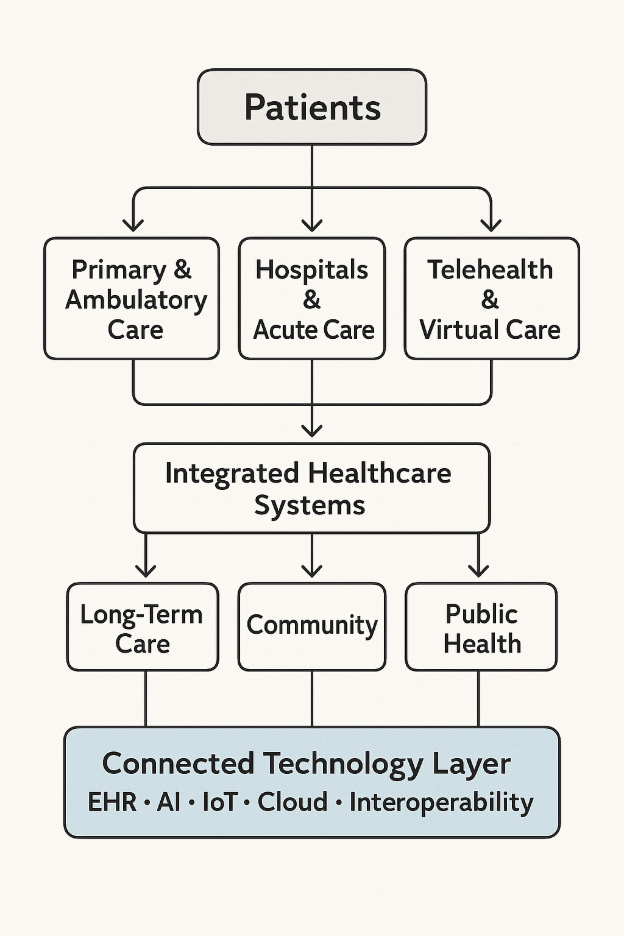
How Technology Is Transforming Healthcare Delivery
Technology is not a separate category of healthcare delivery; it is the force reshaping all of them. Digital transformation in healthcare is connecting every type of system, turning isolated care events into continuous health experiences.
1. Primary Care: From Reactive to Preventive
Electronic Health Records (EHRs) give clinicians immediate access to patient histories, lab results, and prescriptions. Combined with decision-support systems, they help providers make informed choices and detect risks early.
Mobile applications and automated reminders encourage patients to follow care plans, get vaccinations on time, and maintain wellness.
Impact: Preventive care becomes proactive, measurable, and data-supported.
2. Hospitals: Smart Operations and AI-Driven Insights
Hospitals now rely on integrated digital systems for nearly every function. Predictive analytics help forecast admissions and optimize staffing. AI-powered diagnostics assist radiologists and pathologists in detecting patterns invisible to the human eye.
Smart sensors and IoT devices ensure that critical equipment is available and functioning. This transformation enhances safety, efficiency, and patient throughput.
Research from the National Institutes of Health (NIH) shows that AI-driven diagnostic systems are already enhancing clinical efficiency and accuracy across modern hospital environments.
Impact: Reduced errors, improved decision-making, and more efficient resource utilization.
3. Integrated Systems: Interoperability as the Foundation
For integrated healthcare delivery systems, interoperability determines success. Data integration through FHIR standards and secure APIs allows patient information to move freely between providers, payers, and pharmacies.
With unified dashboards, care teams can coordinate across locations, eliminating redundancy and improving patient experience.
Impact: Seamless communication, better outcomes, and stronger collaboration across the continuum of care.
4. Long-Term Care: Remote Monitoring and Real-Time Support
Connected devices such as wearables and home health sensors transmit data directly to clinicians. Early detection of irregularities allows care teams to intervene before hospitalization becomes necessary.
For patients with chronic conditions, digital care plans and video check-ins reduce travel and improve adherence.
Impact: Continuous oversight and personalized long-term support that blends clinical expertise with home comfort.
5. Community Health: Smarter Public Health Infrastructure
Public health agencies use analytics platforms to track population-level data and predict disease trends. Cloud-based systems support rapid response to emerging threats and efficient distribution of vaccines or supplies.
Impact: Data-driven planning and faster response during health crises.
6. Telehealth: Expanding the Reach of Care
What began as video consultations has evolved into a full-scale digital ecosystem. Wearables measure real-time vitals, AI triage tools guide patients to appropriate care, and digital follow-ups ensure continuity.
For patients with mobility challenges or chronic conditions, telehealth reduces barriers and supports long-term engagement.
Impact: Expanded access, better follow-through, and increased patient satisfaction.
The Road Ahead: Toward Connected Healthcare Systems
All these advances point toward a future where healthcare is no longer defined by geography or hierarchy but by connection. The next decade will see connected healthcare systems that combine clinical intelligence with personalized engagement.
Care will move fluidly between in-person visits, home environments, and digital touchpoints. Data will flow securely across organizations, making the healthcare experience more coordinated and transparent for patients and providers alike.
Challenges to Address
While technology creates new opportunities, several barriers remain:
- Lack of full interoperability between systems.
- Unequal access to digital tools or connectivity.
- Data privacy and cybersecurity risks.
- Training gaps and cultural resistance within healthcare teams.
Addressing these will determine how quickly healthcare systems can evolve from fragmented to fully connected.
Conclusion
The types of healthcare delivery systems may vary in design, but they are now bound by a single thread — technology that unites people, data, and decisions across the continuum of care.
From digital-first primary care to AI-assisted diagnostics and connected home monitoring, the shift toward intelligent, coordinated systems is transforming how healthcare is experienced. The next leap lies not just in adopting technology, but in engineering it around the unique workflows, compliance requirements, and patient outcomes that define each organization.
At Nalashaa, our custom healthcare software development services help providers, payers, and HIT vendors build secure, interoperable, and scalable platforms that power modern care delivery. Whether it’s EHR integration, telehealth enablement, or connected care application design, we tailor every solution to the realities of healthcare operations.
If your organization is exploring ways to modernize or connect its delivery systems, our team can help.
Connect with us at info@nalashaa.com to start a conversation about building technology that works as seamlessly as the care you deliver.