Why ICD Still Trips Leaders Up
For something as established as the International Classification of Diseases, you would expect smooth sailing by now. Yet every October, when the latest ICD-10-CM and ICD-10-PCS updates go live in the US, hospitals, payers, and vendors scramble to catch up. Training sessions are rushed, EHR prompts break, and claims bounce back because codes don’t align.
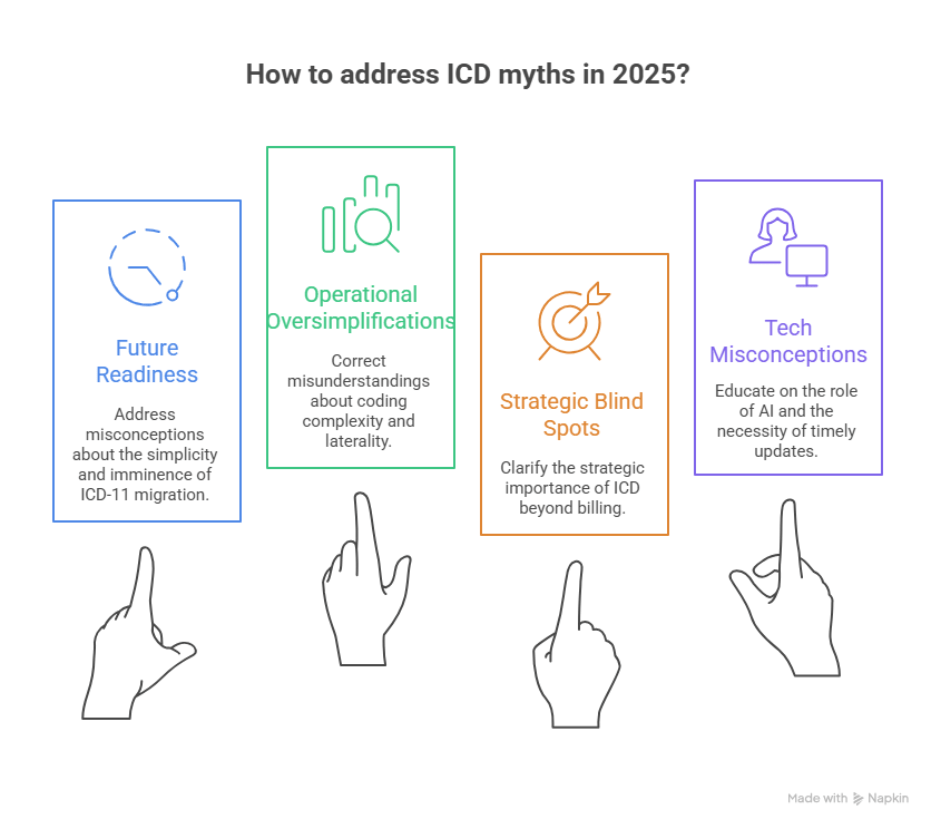
The bigger problem isn’t just the code updates. It’s the myths that executives quietly accept about ICD. Myths like “ICD is only for billing” or “ICD-11 is around the corner, so we can wait.” These assumptions shape budgets, workflows, and technology roadmaps. Left unchecked, they drain revenue, distort analytics, and expose organizations to compliance risk.
This blog breaks down the most common ICD myths we still hear from providers, payers, and health IT vendors. Each one matters because it affects how leaders fund data strategy, how systems handle compliance, and how teams stay audit-ready. The goal is not to nitpick coders but to reset leadership’s view of ICD as more than a back-office function.
Myth 1: ICD-11 is about to replace ICD-10 in the US
The belief: Many leaders assume the US is days away from flipping the switch to ICD-11. After all, the WHO declared it effective in 2022, and countries like Australia and Canada are already exploring migration.
The reality: The US remains firmly on ICD-10-CM for diagnoses and ICD-10-PCS for inpatient procedures. These code sets are updated every October by CMS and CDC/NCHS. No official timeline exists for an ICD-11 transition. In fact, federal agencies are still in exploration mode, and a shift of this scale will take years of testing, dual coding, and payer alignment.
Why it matters: Planning for ICD-11 as if it is imminent wastes budget and distracts teams from the real, yearly ICD-10 updates that directly affect reimbursement. CXOs should focus on building an annual update playbook rather than chasing a speculative ICD-11 timeline.
Myth 2: ICD is just for billing
The belief: Some executives still treat ICD as a billing code dictionary, a job for back-office teams with little strategic relevance.
The reality: ICD codes drive far more than claims. They feed risk adjustment models, population health analytics, quality reporting, and epidemiological tracking. When codes are wrong, it doesn’t just slow cash flow — it warps the very data leaders use to design care strategies and negotiate payer contracts. WHO calls ICD the global health information standard, not a billing afterthought.
Why it matters: Misunderstanding ICD as “just billing” blinds leadership to its impact on revenue integrity and compliance. It also creates silos, where clinical and financial teams don’t share ownership of data quality. Leaders need to elevate ICD accuracy as a board-level KPI tied to both reimbursement and strategy.
Myth 3: ICD-10-CM and ICD-10-PCS are interchangeable
The belief: Because they share the “ICD-10” label, some assume CM and PCS are variations of the same thing, or that coders can use them interchangeably.
The reality: They serve completely different purposes. ICD-10-CM is the diagnosis classification system. ICD-10-PCS is an inpatient procedure coding system unique to the US, built on a seven-character structure with its own logic and guidelines. Misusing them leads to denied claims, compliance issues, and flawed analytics.
Why it matters: Confusion between CM and PCS is not just a coding error — it’s a leadership oversight. If training budgets, EHR workflows, or audit programs don’t distinguish the two, executives risk systemic errors that undermine reimbursement and expose the organization to penalties.
Myth 4: One diagnosis code per visit is enough
The reality: ICD-10-CM demands specificity. A patient encounter may require multiple diagnosis codes — covering complications, laterality, comorbidities, or sequela. The system was designed to paint a complete picture of the patient’s condition. A single generic code hides critical details, undermining DRG assignment and risk scoring.
Why it matters: Under-coding does not just reduce reimbursement. It distorts quality metrics, weakens analytics, and can misrepresent the true burden of disease in your population. Executives should view “one code per visit” as a red flag for both compliance risk and data quality.
Myth 5: Z-codes for social determinants are optional
The belief: Because payers don’t always require them, many organizations skip Z55–Z65 codes that capture social determinants of health (SDOH), assuming they add little value.
The reality: Z-codes are increasingly critical. They document food insecurity, housing instability, transportation barriers, and other non-clinical drivers of health. CMS, NCQA, and professional associations continue to encourage their use, and new Z-codes are introduced each year during ICD updates. Capturing them improves care coordination and positions organizations for value-based contracts that factor in social risk.
Why it matters: Ignoring Z-codes blinds analytics teams to patient needs and undercuts care management funding opportunities. For CXOs, the takeaway is clear: train front-line teams to capture SDOH data and build coding policies that treat Z-codes as essential, not optional.
Myth 6: Any AI auto-coder can replace expert coders
The belief: With AI tools flooding the market, some leaders assume they can automate coding entirely and cut headcount.
The reality: AI can accelerate abstraction and suggest codes, but it cannot replace expert judgment. Models inherit bias and errors from their training data, and without human oversight, they can miscode encounters at scale. Regulators are already signaling that AI-assisted coding still requires audit trails, version control, and human review.
Why it matters: Treating AI coders as a full replacement exposes organizations to denials, compliance penalties, and liability under false claims laws. The smarter approach is to deploy AI as an assistant that handles repetitive coding while certified coders review, validate, and manage exceptions.
Computer-assisted coding (CAC) tools set the stage for today’s AI coders. Our [blog on CAC implementation] shows the early challenges that still matter now.
Myth 7: Mapping SNOMED CT to ICD is straightforward
The belief: Since both are clinical vocabularies, leaders sometimes assume SNOMED CT concepts map neatly into ICD codes.
The reality: SNOMED CT is a clinical terminology built for precision at the point of care. ICD is a classification system built for reporting and reimbursement. Many SNOMED concepts map to multiple ICD codes, and context often determines the correct choice. For example, a single SNOMED entry for “diabetes with complications” might require several ICD codes depending on the organ system affected.
Why it matters: If mappings are treated as one-to-one, analytics and claims can be consistently wrong across an entire population. For executives, this is not an IT nuisance — it’s a data governance issue that affects compliance and decision-making.
Myth 8: Upcoding is just a coder issue
The belief: Upcoding gets blamed on coders “choosing higher-paying codes” to maximize revenue.
The reality: Coding problems often originate upstream. Poorly designed EHR templates, default settings, or vague documentation can push encounters toward higher severity levels without intent. That places the organization at audit risk, even if coders are following the documentation they receive.
Why it matters: Upcoding is a leadership problem, not just a coding one. CXOs should be auditing clinical documentation workflows and EHR templates as carefully as coder output. Otherwise, they risk financial penalties and reputational damage from investigations.
Myth 9: Laterality and staging are minor details
The belief: Small details like left vs right, initial vs subsequent encounter, or disease stage are seen as clinical nuance that doesn’t affect the bottom line.
The reality: These details are often the difference between an accurate ICD-10-CM code and a generic one. Missing laterality or stage leads to denials, lower reimbursement, and reduced clinical fidelity. Payers use these fields for risk adjustment, and regulators expect them for accurate reporting.
Why it matters: Overlooking laterality or staging signals weak documentation discipline. For leadership, this is a compliance and revenue integrity gap. Investing in training and edits that catch missing details pays off by preventing systemic data erosion.
Myth 10: External cause codes are unnecessary
The belief: Because they rarely drive reimbursement, many leaders assume external cause codes (like “fall from ladder” or “accidental poisoning”) are irrelevant.
The reality: External cause codes provide essential context for injuries and poisonings. They are used in state-level reporting, trauma registries, and quality programs. Payers may also require them for specific claims. When missing, the data gaps ripple into public health tracking and patient safety analytics.
Why it matters: Treating these codes as optional weakens compliance and undermines participation in reporting programs. Leaders should ensure systems prompt for external cause details where required, avoiding both penalties and gaps in safety metrics.
Myth 11: Risk adjustment means “more codes”
The belief: Some executives think risk adjustment success is about capturing as many codes as possible to drive higher risk scores.
The reality: Risk models such as HCC rely on specificity and clinical validation, not volume. Unsupported or vague codes can trigger audits and penalties, while precise codes linked to solid documentation strengthen both reimbursement and care management funding. More codes without accuracy equals more liability.
Why it matters: Over-coding in risk adjustment contracts exposes the organization to financial clawbacks. Executives must push for documentation improvement initiatives that favor specificity and evidence, not volume for its own sake
Myth 12: ICD updates are ad hoc and can be delayed
The belief: Updates can be slotted in when IT and HIM teams “have time,” since most changes are incremental.
The reality: ICD-10-CM and ICD-10-PCS updates follow a strict annual cycle, effective October 1. CMS and CDC publish updates months in advance, and payers expect immediate compliance. Delaying implementation can result in denials, rejected claims, and misaligned reporting.
Why it matters: Missing the update window creates systemic disruption across the revenue cycle, reporting, and analytics. CXOs should treat ICD updates as a fixed program milestone, with budget, ownership, and testing built in each year.
ICD-10-CM updates happen on a fixed annual cycle. Our [guide to FY 2024 ICD-10-CM changes] offers a detailed look at how these updates shape compliance and billing.
Myth 13: ICD-11 will be a simple lift
The reality: ICD-11 is structurally very different. It uses digital architecture, allows multiple coding layers, and changes how conditions are grouped. Transitioning would touch payment logic, quality reporting, analytics, benefit design, and every contract that references ICD. Even countries already implementing ICD-11 are phasing it in slowly. The US has no official migration date, but when it comes, it will demand years of preparation.
Why it matters: Underestimating the complexity leads to budget shocks and failed pilots. Executives need to begin with impact assessments, vendor readiness checks, and dual-coding strategies well before federal mandates arrive.
Myth 14: SDOH Z-codes are static
The belief: Once teams learn the Z-codes for social determinants of health, they can use the same list indefinitely.
The reality: Z-codes evolve. New codes are added during annual ICD updates to capture emerging social risk factors. Federal agencies and professional associations are actively expanding these categories as SDOH becomes a bigger part of value-based care. Using outdated Z-code lists creates blind spots in both reporting and patient care.
Why it matters: Stale SDOH coding means leaders miss opportunities for funding, analytics accuracy, and care coordination. Executives should ensure Z-code lists are refreshed every October and staff are trained on the changes.
Conclusion
ICD is the backbone of revenue integrity, risk adjustment, and healthcare analytics. The myths around ICD — from “one code is enough” to “ICD-11 will be easy” — are not harmless misunderstandings. They shape budgets, workflows, and compliance risk at the enterprise level.
Leaders who address these misconceptions early protect both revenue and reputation. More importantly, they create reliable data that supports strategy, contracts, and patient care.
Executive Checklist
- Assign an accountable owner for yearly ICD-10 updates (October cycle).
- Audit EHR templates and workflows for hidden upcoding risks.
- Treat Z-codes for SDOH as essential for analytics and contracts.
- Run AI-assisted coding with human oversight and audit logs.
- Start ICD-11 readiness assessments now, even without a mandate.
The organizations that thrive will be those that stop treating ICD as a static code book and start managing it as a strategic asset. Connect with us at info@nalashaa.com to discuss your challenges.