Hospitals today run on a strange mix of the old and the new. A claims clerk still keys data into green-screen interfaces that look like they belong in the 90s, while in another department, an AI tool drafts discharge summaries in seconds. Leadership teams hear pitches about RPA for quick wins, AI for smarter predictions, and now Agentic AI as the future of autonomous operations. The buzzwords pile up faster than the budgets to fund them.
Each of these technologies has a role. RPA delivers consistency in repetitive tasks. AI recognizes patterns and predicts outcomes. Agentic AI goes further, orchestrating workflows that act across systems without waiting for step-by-step instructions. The real challenge isn’t choosing a winner. It’s knowing how to match the right level of automation to the right problem without getting lost in hype or missing real opportunities.
This article breaks down the differences, explores where each approach fits in healthcare, and offers a practical framework for decision-makers to avoid costly detours on the road to smarter automation.
RPA in Healthcare
Every healthcare leader has heard some version of this promise: “Let the bots do the boring work.” That is exactly what Robotic Process Automation (RPA) was built for. Instead of a staff member logging into three systems, copying data from one, and pasting it into another, an RPA bot follows the same clicks and keystrokes with perfect consistency.
In healthcare, RPA has become the quiet backbone of revenue cycle operations. Eligibility verification, claim status checks, patient scheduling, and data transfers between payer portals and EHRs are all prime candidates. These are predictable, rule-based tasks that eat up thousands of staff hours each month but rarely require judgment or creativity.
The attraction is obvious: quick wins without large infrastructure changes. Bots can be deployed to work over existing systems, even those old green-screen applications, without waiting for modern APIs or vendor upgrades. Hospitals often see immediate savings in staff time and error reduction once they automate the low-hanging fruit.
But RPA has limits. The moment a process changes, or an unexpected variation appears, bots stumble. A missing field or a new screen layout can derail an entire workflow. They do not adapt or learn, which means ongoing maintenance becomes part of the equation. RPA is effective at removing repetitive drudgery, but it is not designed to think ahead or make sense of messy, unstructured data.
In short, RPA is the dependable workhorse of automation: tireless, consistent, and reliable for what it does best. Just do not expect it to carry the load of higher-order decisions or predictive insight.
AI in Healthcare
If RPA is about following instructions, AI is about recognizing patterns and making sense of data that humans could never process at scale. It is the difference between a clerk copying fields line by line and an algorithm scanning thousands of claims to predict which ones are likely to be denied.
AI has slipped into healthcare in subtle but powerful ways. Natural language processing tools help convert free-form physician notes into structured documentation. Machine learning models scan historical claims data to identify denial risks before they are submitted. Image recognition algorithms assist radiologists by flagging abnormalities in scans that deserve a closer look. Each of these examples goes beyond rule-following into the realm of insight.
The strength of AI is that it thrives in messy, unstructured environments where RPA fails. Doctors do not all write notes in the same way. Insurance carriers apply policies with different conditions. Patients present with unique combinations of history and symptoms. AI can sift through this complexity, find patterns, and provide actionable recommendations.
Yet the promise comes with weighty considerations. AI systems demand large, high-quality datasets to train effectively, and in healthcare, clean data is often in short supply. Transparency is another challenge. A predictive model may flag a claim as “high risk,” but unless the reasoning is explainable, billing teams may hesitate to trust it. Regulators are watching closely as well, requiring that AI in healthcare meets strict standards for accuracy, fairness, and patient safety.
AI is not a replacement for human expertise. It is a force multiplier that turns overwhelming amounts of data into signals that clinicians and administrators can act on. When used carefully, it can reduce errors, lower costs, and improve outcomes. But without strong governance and clear accountability, it risks becoming another black box in a system already burdened by complexity.
Agentic AI in Healthcare
If RPA handles routine and AI interprets patterns, Agentic AI takes a step further. It does not just respond when asked. It plans, decides, and acts across multiple systems to achieve a goal. Think of it less as a tool and more as a teammate that can manage entire workflows on its own.
Healthcare has begun to see early examples. At Athenahealth, Agentic AI agents are being tested to triage and respond to messages, draft patient follow-ups, and offload administrative burden from care teams. In surgical departments, generative and agentic models are used together to automatically create post-operative instructions based on a surgeon’s notes. In the revenue cycle, experimental agents are emerging that not only flag denial risks but also prepare corrected claims for resubmission without human intervention.
The shift is profound. Unlike RPA, which waits for predefined rules, or AI models that predict outcomes, Agentic AI can orchestrate multi-step processes. A patient engagement agent, for example, could detect a missed appointment, reschedule automatically, send reminders, and escalate to a live staff member only if the patient does not respond. It is a new level of autonomy that promises to relieve staff from routine oversight.
Of course, autonomy brings risk. Agentic AI requires tight guardrails to prevent errors from cascading. Healthcare data is sensitive, and the idea of a system making decisions without human approval raises regulatory and ethical questions. Oversight, transparency, and escalation protocols are not optional; they are essential.
Agentic AI is not science fiction. It is already being piloted in hospitals and payer organizations. But adoption will depend on whether healthcare leaders can strike a balance between bold innovation and cautious governance. Those who succeed will unlock a model where automation does more than save time; it actively drives better care and operational outcomes.
RPA vs AI vs Agentic AI
Understanding how these three approaches differ is the first step to making the right investment. RPA works well where tasks are repetitive and predictable. AI adds intelligence where data is complex and unstructured. Agentic AI moves beyond both by handling multi-step processes with a degree of autonomy.
| Aspect | RPA | AI | Agentic AI |
| Nature | Rule-based automation that mimics human clicks and keystrokes | Learns from data to recognize patterns, classify, or predict outcomes | Acts as an autonomous agent that can plan, decide, and carry out multi-step workflows |
| Best for | Adaptive, proactive, and orchestrates across multiple systems without waiting for manual prompts | Handles unstructured data, predictive insight, and supports decision-making | Patient engagement, claims resubmission, intelligent scheduling, proactive care coordination |
| Strengths | Fast deployment, lower cost, consistent performance | Eligibility checks, claim submissions, form filling, and routine data transfers | Adaptive, proactive, orchestrates across multiple systems without waiting for manual prompts |
| Weaknesses | Breaks easily when processes change, limited to structured tasks | Requires large, clean datasets, explainability issues, and regulatory scrutiny | Higher complexity, governance required, risks if oversight is weak |
| ROI potential | Quick wins with measurable savings on repetitive tasks | Greater long-term efficiency and accuracy improvements | Transformative if scaled responsibly, highest potential for strategic impact |
The progression is clear. RPA creates efficiency, AI builds intelligence, and Agentic AI introduces autonomy. The decision is not which one to choose in isolation, but how to layer them in a way that fits your organization’s readiness and goals.
Where RPA, AI, and Agentic AI Fit in Healthcare
Not every hospital or payer needs the same level of automation. The right choice depends on the size of the organization, the maturity of its IT systems, and the problems that need solving first.
RPA for quick relief
Smaller clinics and physician practices often start with RPA. Tasks like insurance eligibility checks, prior authorization submissions, or routine claim status inquiries are repetitive and rules-based. Automating them can cut hours of staff time each week and reduce the risk of manual errors. The return shows up quickly without requiring heavy data infrastructure.
AI for smarter operations
Mid-sized hospitals and health systems are beginning to see value from AI. Predictive denial management, automated clinical documentation, and coding assistance are practical areas where machine learning delivers results. According to Change Healthcare, claim denial rates in the U.S. average 10 to 15 percent, costing providers billions annually. AI models that flag high-risk claims before submission can make a measurable impact on revenue cycle performance. On the clinical side, natural language processing tools help reduce the documentation load that drives physician burnout.
Agentic AI for system-wide orchestration
Large health systems and payer organizations are experimenting with Agentic AI to move from efficiency to autonomy. For example, some pilots have shown that autonomous agents can not only identify a denied claim but also generate a corrected resubmission draft and route it for approval. In patient engagement, agentic models are being tested to manage the entire process of scheduling, reminders, and follow-ups without human intervention unless escalation is needed. Athenahealth has reported early results from agentic pilots that offload message triage and draft responses for care teams, freeing clinicians to focus on patient interaction.
The progression is less about technology hype and more about matching ambition to readiness. Smaller organizations find relief in RPA, mid-sized ones gain leverage from AI, and the largest players explore agentic approaches to orchestrate across departments.
Key Considerations and Challenges
Healthcare automation cannot be judged only by what the technology promises. The real test lies in whether it works within the constraints of regulation, trust, and day-to-day operations.
Data quality and availability
AI and agentic models need large, accurate datasets to train effectively. In healthcare, data is often scattered across EHRs, billing systems, lab platforms, and payer portals. Incomplete or inconsistent records can undermine the reliability of predictions. Without a solid data foundation, advanced automation efforts stumble.
Compliance and security
HIPAA, HITECH, and emerging AI regulations set strict boundaries on how patient information is handled. RPA bots may seem simple, but if they are not monitored, they can mishandle protected health data. AI models must also be validated for accuracy and fairness. Agentic AI raises additional questions about transparency and accountability, since it acts with a degree of independence. Leaders cannot adopt these tools without a compliance-first strategy.
Trust and explainability
A denial prediction model that cannot explain why a claim is flagged is less likely to be trusted by billing teams. Clinicians hesitate to rely on AI-generated summaries if they cannot see the reasoning behind them. Agentic systems amplify this concern because their workflows span multiple steps. Building trust requires explainable outputs, human oversight, and clear escalation paths.
Change management
Automation changes the way staff work. RPA may remove repetitive data entry, but staff must learn to monitor and manage bots. AI reduces documentation effort, but clinicians need training to adopt new workflows. Agentic AI will require even greater cultural adjustment, as employees move from task execution to supervising autonomous systems. Without structured change management, adoption will face resistance.
Ongoing maintenance
None of these technologies is “set and forget.” RPA bots break when interfaces change. AI models drift as data evolves. Agentic AI agents must be continuously tested for safety, accuracy, and compliance. Sustainable automation requires governance structures that treat these systems as living parts of the organization, not one-time projects.
The opportunity is clear, but so are the risks. Leaders who approach automation with discipline and governance are more likely to realize value without creating new problems.
Decision Framework – Choosing the Right Path
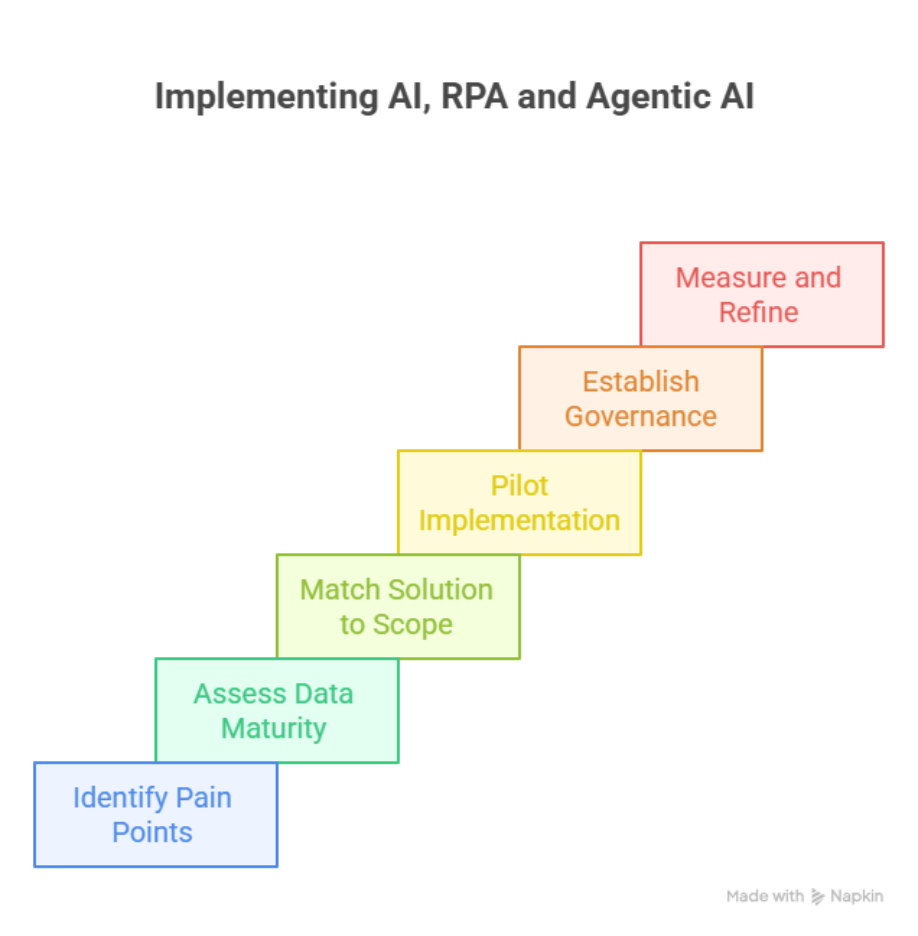
The choice between RPA, AI, and Agentic AI is not about picking a single winner. It is about aligning the right tool with the right challenge, while considering your organization’s readiness and appetite for risk.
Step 1: Map your current pain points
Start with the workflows that drain the most time or create the highest error rates. For many providers, this means eligibility checks, prior authorizations, or repetitive claims processes. Identifying these bottlenecks is the foundation for deciding where automation should begin.
Step 2: Assess your data maturity
RPA requires structured and predictable inputs, while AI and Agentic AI depend on large and reliable datasets. If your records are fragmented across multiple systems or filled with inconsistencies, investing in advanced models before fixing data quality will limit results.
Step 3: Match the solution to the scope
- For rule-driven, repetitive tasks: RPA is sufficient and offers quick wins.
- For prediction, classification, or working with unstructured data: AI is a better fit.
- For multi-step, dynamic workflows that span departments: Agentic AI holds promise.
Step 4: Pilot before scaling
Launching a small pilot reduces risk and builds internal support. An RPA bot in claims processing or an AI model for denial prediction can deliver measurable results quickly. Pilots also highlight integration issues before larger investments are made.
Step 5: Establish oversight and governance
Automation without oversight creates new risks. Define who monitors RPA bots, how AI predictions are validated, and when Agentic AI agents must escalate to human decision-makers. Governance should include compliance officers, IT leaders, and clinical representatives.
Step 6: Measure and refine
Set clear KPIs such as denial reduction rates, documentation time saved, or improved patient throughput. Use these metrics to refine automation efforts and justify expansion to other areas of the organization.
The right framework ensures automation investments are not driven by hype but by measurable outcomes. Incremental progress, paired with disciplined oversight, creates the foundation for moving from RPA to AI and eventually to Agentic AI with confidence.
Conclusion
Healthcare is caught between old systems that demand manual effort and new technologies that promise speed, accuracy, and insight. RPA, AI, and Agentic AI are not competitors fighting for dominance. They are stages in a maturity curve that can be aligned to the realities of each organization. RPA clears the repetitive clutter, AI brings intelligence to messy data, and Agentic AI pushes toward autonomy where workflows manage themselves.
At Nalashaa, we help providers, payers, and healthcare IT vendors map the right automation strategy to their goals. Our healthcare automation solutions cover everything from RPA bots that stabilize revenue cycle tasks to AI that predicts denials to agentic pilots that orchestrate complex workflows.
Ready to see which automation layer fits your organization? Let’s start with an assessment of your workflows and data readiness. Connect with us at info@nalashaa.com
Latest posts by Priti Prabha (see all)
- Population Health Analytics for Healthcare Payers - January 15, 2026