Interoperability in healthcare refers to the capability of different health information systems, applications, and devices to seamlessly exchange and interpret patient data for better collaboration among healthcare providers. Clinical data interoperability ensures patient information can move freely between different electronic health record (EHR) systems, supporting informed clinical decisions and coordinated patient care.
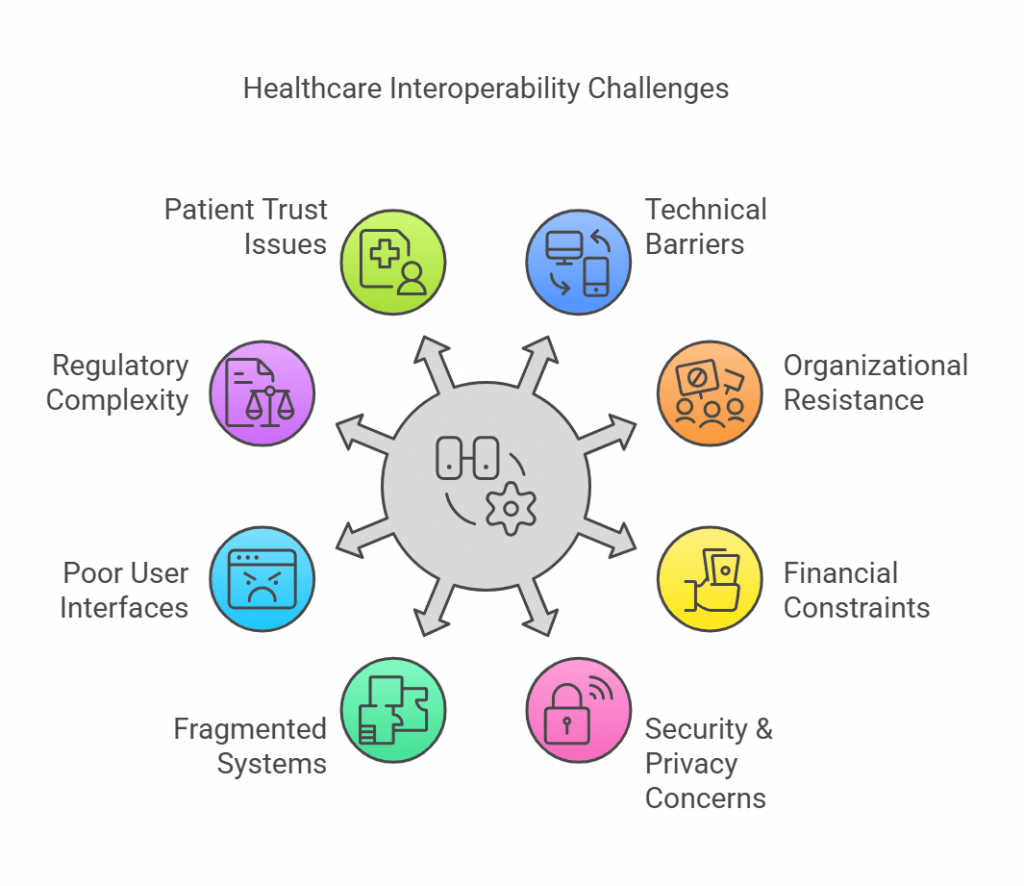
However, achieving interoperability is inherently complex. Despite its benefits, healthcare organizations frequently struggle with the lack of interoperability in healthcare due to technological, organizational, and cultural barriers. As healthcare becomes increasingly digitalized, these hurdles must be addressed to realize the full potential of interconnected patient care.
1. Technical Challenges
Technical challenges form the foundational barrier to achieving interoperability in healthcare. Issues rooted in the technology itself must first be addressed to enable efficient data exchange.
Lack of Standardization
A primary technical challenge is the lack of universally accepted standards among EHR systems. Vendors often use proprietary formats, causing compatibility issues when data needs to be shared. Without standardized methods for encoding and exchanging data, providers experience substantial obstacles, resulting in fragmented patient records.
Data Format Inconsistencies
Varied data structures across healthcare systems disrupt the flow of clinical information. Even minor differences in data representation or coding schemes can lead to misinterpretation or data loss during exchanges. This inconsistency complicates the aggregation and analysis of patient data, negatively impacting patient outcomes and care quality.
Legacy Systems
Many healthcare providers still rely on legacy systems designed before widespread interoperability became essential. These outdated platforms typically lack the necessary features or adaptability to integrate effectively with modern, interoperable solutions, severely restricting clinical data interoperability. Updating or replacing legacy systems often involves substantial financial investment and complex technical undertakings, further discouraging organizations from moving forward.
Technical Complexity
Integrating multiple technology platforms from various vendors introduces more hurdles. Interoperability demands specialized knowledge to maintain system compatibility and ensure secure data exchange. This complexity grows as more stakeholders and varied technologies become involved, raising the risk of integration failures and downtime.
2. Organizational and Cultural Challenges
Beyond technical issues, organizational culture and practices influence the success of interoperability initiatives. Addressing these non-technical barriers is equally vital to ensure sustained adoption and effective utilization of interoperable systems.
Resistance to Change
Healthcare professionals accustomed to existing workflows and systems often resist the adoption of new interoperable technologies. This resistance stems from uncertainty about new processes, potential disruptions to daily tasks, and concerns regarding training and system reliability. Without addressing these concerns through effective communication and training, resistance can significantly delay or halt interoperability initiatives.
Lack of Coordination and Collaboration
Interoperability requires robust collaboration across multiple stakeholders, including healthcare providers, IT departments, and vendors. However, organizational silos often prevent effective communication, leading to disconnected initiatives and isolated pockets of technology implementation. Such fragmentation makes holistic interoperability exceedingly challenging.
Patient Identification and Matching
Accurately matching patient records across different healthcare systems is another critical challenge. Variations or errors in patient information, such as names or addresses, complicate the matching process, increasing risks of clinical errors and miscommunication. Implementing reliable patient identification strategies remains essential yet difficult due to inconsistent practices and standards.
Data Governance
Effective data governance involves establishing clear policies for data accuracy, integrity, and secure handling. Unfortunately, inadequate governance frameworks often compromise data quality and trust among stakeholders. The absence of well-defined data governance guidelines leads to uncertainty about data sharing responsibilities, privacy protocols, and regulatory compliance, impeding interoperability efforts.
3. Financial and Resource Challenges
Financial and resource limitations influence healthcare interoperability. Allocating sufficient resources for interoperability initiatives often competes with other pressing organizational priorities, hindering the adoption of advanced technologies.
High Implementation Costs
The adoption of interoperable systems involves substantial initial investments, including hardware, software, and training expenses. Such high upfront costs can deter organizations, especially smaller providers, from pursuing interoperability projects.
Budget Constraints
Healthcare organizations frequently face tight budgets, limiting the resources available for comprehensive interoperability projects. Budgetary limitations can result in partial implementation, leading to fragmented and ineffective interoperability solutions.
Lack of Skilled Personnel
There is a notable shortage of qualified professionals with the expertise needed to implement, manage, and maintain interoperable systems. This scarcity often results in increased operational challenges and reliance on external expertise, raising overall costs and complexity.
4. Security and Privacy Challenges
Increased data sharing across platforms intensifies concerns around data protection and regulatory compliance, which adds complexity to interoperability.
Data Security Breaches
Enhanced interoperability can inadvertently increase vulnerability to cyber threats, potentially exposing sensitive patient information. Healthcare organizations must implement robust cybersecurity measures, which demand additional resources and continuous vigilance.
Regulatory Compliance
Compliance with stringent regulations, such as HIPAA, introduces additional complexity when exchanging patient data across different systems. Failure to meet regulatory standards can lead to severe penalties, heightening caution, and sometimes limiting interoperability efforts.
Data Privacy
Maintaining patient confidentiality while enabling data sharing is a balancing act. Clear privacy protocols and secure handling practices must be established, yet these requirements can significantly slow down interoperability progress if not effectively managed.
5. Fragmented Systems and Data Silos
Fragmentation within healthcare organizations poses a significant barrier to interoperability. Departments often operate in isolation, using separate technologies, processes, or systems, leading to disconnected information flows and incomplete patient records.
Isolated EHR Systems
Healthcare facilities frequently use multiple EHR systems across departments, each with proprietary data formats or incompatible interfaces. This isolation restricts internal data sharing, resulting in duplicated effort, inconsistent patient data, and compromised patient care quality.
Data Silos
Data silos arise when data is stored in isolated repositories without clear guidelines or methods for integration. Such silos hinder the sharing of valuable clinical insights, limit comprehensive analysis of patient health, and complicate clinical decision-making. Breaking down these data silos is essential yet challenging due to proprietary interests and technical incompatibilities.
6. User Experience and Interface Challenges
User experience plays a critical role in how effectively interoperable systems are adopted and utilized in healthcare environments. Poorly designed systems can hinder healthcare professionals’ productivity and negatively impact patient care.
Poor User Interfaces
Complex or unintuitive interfaces can frustrate healthcare workers, causing delays in data entry and retrieval. Systems that aren’t user-friendly may lead to incomplete patient records or data entry errors, undermining the benefits of interoperability.
User Adoption and Training
Successful implementation of interoperable systems requires extensive training and user support. Often, healthcare organizations underestimate these needs, leading to inadequate training and low adoption rates. Without proper support, users may revert to older systems, limiting the effectiveness of interoperability investments.
7. Policy and Regulatory Challenges
Healthcare interoperability must align with evolving regulations and policies. Navigating these complexities is challenging but crucial to achieving widespread interoperability.
Varying Regional Regulations
Different regions and states have distinct rules governing healthcare data exchange. These regulatory differences add complexity to interoperability initiatives, particularly for organizations operating across multiple jurisdictions. Aligning technology and processes with varied compliance requirements demands significant administrative effort.
Lack of Harmonized Policies
Currently, there’s no universally harmonized policy framework for healthcare interoperability. Inconsistencies between policies at the local, state, and federal levels result in uncertainty and impede the development of standardized data exchange practices. Creating harmonized policies that bridge jurisdictional gaps is essential to streamline interoperability efforts.
8. Patient Trust and Consent Challenges
Patient consent and trust are critical yet frequently overlooked aspects of interoperability. Healthcare interoperability initiatives must adequately address patient perspectives to ensure robust adoption and ethical data use.
Patient Reluctance to Share Data
Patients often express hesitation in sharing their health data across multiple platforms or providers due to privacy concerns. This reluctance leads to incomplete patient records, limiting the effectiveness of interoperability initiatives and clinical decision-making.
Complex Consent Management
Managing patient consent across multiple systems and organizations is challenging, particularly when regulations and patient preferences vary. The complexity of consent management increases administrative burdens, creates confusion among providers, and can slow data sharing, negatively impacting patient care coordination.
Conclusion
Addressing EHR interoperability challenges requires collaboration among technology providers, healthcare organizations, policymakers, and patients. Overcoming technical, cultural, financial, security, policy-related, and patient trust barriers demands comprehensive strategies, targeted investments, and sustained commitment.
Nalashaa Solutions specializes in navigating these interoperability complexities. With extensive expertise in clinical data interoperability, we help healthcare organizations overcome barriers such as standardization issues, legacy system integration, data governance, and consent management. Our healthcare interoperability solutions promote secure, efficient data exchange and enhance operational effectiveness.
To understand how Nalashaa Solutions can facilitate your journey towards seamless interoperability, connect with us at info@nalashaa.com.
Latest posts by Priti Prabha (see all)
- ONC HTI 1 Final Rule and Certified APIs: A Complete Guide - February 19, 2026