In 2015, CMS launched the Interoperability Roadmap, a 10-year initiative to create a unified health data-sharing ecosystem across the U.S. he U.S. As we approach 2025, the roadmap is reaching its final phases. Recent advancements like TEFCA 2.0, the Interoperability and Prior Authorization rule, and the integration of Qualified Health Information Networks (QHINs) are paving the way for a cohesive, nationwide framework. These steps bring CMS closer to achieving a secure data exchange across providers, payers, and patients.
The roadmap’s aim is to enable a healthcare environment where information flows freely, such that providers can make informed decisions for better patient outcomes. This blog explores the roadmap’s goals, recent progress, and its path to achieving full healthcare interoperability by 2025.
The Vision of the CMS Interoperability Roadmap
One of the healthcare interoperability roadmap’s central goals is to establish a learning health system—an environment where every data exchange contributes to continuous healthcare improvement. This vision supports a model where patient data is available for immediate treatment and is also used to analyze trends, personalize care, and improve health outcomes over time.
Collaboration Among Key Stakeholders
Achieving this vision requires the collaboration of multiple stakeholders—healthcare providers, payers, patients, and health IT vendors. Each group plays a role:
- Providers rely on real-time access to patient information for coordinated and informed care.
- Payers contribute by streamlining processes that improve the quality and accessibility of care.
- Patients gain control over their data to analyze the progress of their healthcare journey and make decisions.
- Health IT Vendors are responsible for the systems that make data compatible for sharing in a safe manner.
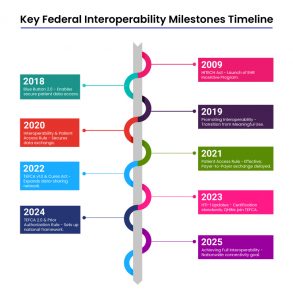
Interoperability Milestones
The Roadmap’s Phased Goals for Interoperability
The CMS interoperability roadmap outlined clear phased goals, each building on the last to ensure secure, accessible, and standardized data exchange across all settings.
Immediate Goals (2015-2017)
The roadmap’s initial phase sets the foundation for interoperability through the ability to send, receive, find, and use priority health data. This phase focused on basic data-sharing standards for efficient communication and connecting healthcare providers for better coordination in patient care.
Mid-Term Goals (2018-2020)
In this phase, the roadmap expanded its scope to include a broader range of data sources and users. Key initiatives aimed at increasing patient access to their health information while streamlining provider workflows. Regulations like the Interoperability and Patient Access rule were introduced to ensure that healthcare systems could securely share, and access patient data as needed.
Long-Term Goals (2021-2024)
The roadmap’s final phase establishes a learning health system where interoperability becomes the norm across all healthcare settings. Goals include real-time access to comprehensive patient data, supporting advanced analytics, and a secure, nationwide data flow. Major milestones, including TEFCA 2.0 and the integration of QHINs.
Policies and Regulations Supporting Interoperability
CMS has introduced two pivotal rules to strengthen interoperability and reduce administrative burdens in healthcare: the CMS Interoperability and Prior Authorization Final Rule and the CMS Interoperability and Patient Access Final Rule.
- CMS Interoperability and Prior Authorization Final Rule
Released on January 17, 2024, this rule prioritizes streamlined access to health information, focusing on improving prior authorization processes. By enhancing data exchange between patients, providers, and payers, this rule helps place patients at the center of their care. It mandates that impacted payers implement data-sharing provisions by January 1, 2026, with extended deadlines for certain API requirements until January 1, 2027, to accommodate stakeholder feedback. - CMS Interoperability and Patient Access Final Rule
This rule mandates the use of standardized APIs to facilitate seamless electronic healthcare data exchange. These APIs allow information flow between patients, providers, and payers, supporting patient access to their data via mobile apps or EHR systems. Additionally, CMS adopted the vocabulary and content standards established in the ONC 21st Century Cures Act final rule, ensuring consistency across platforms for a unified, patient-centered health data ecosystem.
Implementing Guide for CMS Interoperability Rule
The CMS roadmap integrates FHIR standards and the USCDI, supported by specific implementation guides and technical standards.
- API Technology and Implementation Guides (IGs)
Under the CMS Interoperability and Patient Access Final Rule, CMS mandates that Medicare Advantage, Medicaid, CHIP, and Qualified Health Plan issuers implement APIs that meet established technical standards. These APIs facilitate secure data exchange between patients, providers, and payers. The CMS Interoperability and Prior Authorization Final Rule expands on these requirements, introducing APIs for provider, payer-to-payer, and prior authorization data exchange, enhancing patient-centered care and reducing administrative burdens. - FHIR Standards and USCDI
The roadmap incorporates HL7 FHIR Release 4.0.1 as a primary standard, ensuring data consistency and compatibility across health systems. FHIR’s normative resources define how clinical and administrative data can be structured and exchanged, creating a stable foundation for interoperable applications. The US Core Implementation Guide further establishes baseline requirements, defining key data elements and profiles for comprehensive health data sharing, with mandated use of US Core Profiles for all implementations in the U.S. - SMART App Launch and OpenID Connect
CMS recommended theSMART on FHIR framework and OpenID Connect for authentication and authorization. These frameworks enable apps to securely request access to FHIR resources via OAuth 2.0, ensuring that only authorized applications can retrieve sensitive health data. - Da Vinci Project Guides
The roadmap references the Da Vinci Implementation Guides, which provide standardized approaches to data exchange for specific use cases, including:
- PDex: For exchanging clinical information when patients change payers.
- Prior Authorization Support (PAS): Facilitates automated prior authorization requests within EHR systems.
- Coverage Requirements Discovery (CRD): Allows providers to retrieve payer coverage requirements at the point of care.
These IGs help reduce redundancy, streamline processes, and ensure that all stakeholders access health information consistently and securely.
Learning from the Healthcare Interoperability Roadmap
The CMS Interoperability set the stage for significant advancements, while the journey has provided valuable lessons through both achievements and challenges. These insights are pivotal for the next phase of healthcare interoperability.
- Incremental Progress is the Norm
- What Worked: The roadmap introduced milestones like the Interoperability and Patient Access Rule and TEFCA, which provided a foundation for standardizing data exchange.
- The Lesson: True interoperability requires a phased approach, as adopting new standards and aligning diverse stakeholders takes time and effort. Unrealistic timelines can lead to partial implementations.
- Collaboration Among Stakeholders is Crucial
- What Worked: Policies encouraged collaboration between providers, payers, patients, and IT vendors to enable better data exchange.
- The Lesson: Fragmentation among stakeholders often leads to inconsistent implementations. Future initiatives must incentivize deeper collaboration to achieve shared goals.
- Standardization Needs Consistency
- What Worked: The introduction of HL7 FHIR and USCDI laid the base for interoperability.
- The Lesson: Inconsistent adoption of these standards across the healthcare ecosystem limited their impact. Stronger governance and support are required to ensure uniform implementation.
- Balancing Privacy and Accessibility
- What Worked: Privacy frameworks like SMART on FHIR improved security while enabling data access.
- The Lesson: Maintaining the right balance between patient privacy and data accessibility remains a challenge. Regulations must evolve alongside technology to address this.
- User-Centric Solutions Drive Success
- What Worked: Tools like Blue Button 2.0 empowered patients by providing access to their data.
- The Lesson: Complex interfaces and fragmented records reduced usability. Simplified, user-friendly solutions are essential to achieving true patient empowerment.
HTI-2: Building on the Lessons
The Health Data, Technology, and Interoperability (HTI-2) proposed rule directly addresses these lessons, taking a pragmatic approach to healthcare interoperability. Here’s how HTI-2 is designed to overcome the challenges and build on the successes of the roadmap:
- Realistic and Phased Implementation
HTI-2 adopts a phased approach to ensure that stakeholders have sufficient time to adapt. For example, the mandate to adopt USCDI version 4 by 2028 provides a realistic timeline for data element expansion and standardization.
- Enhanced Collaboration Through Regulatory Oversight
The proposed rule provides clearer certification criteria and accountability measures to align providers, payers, and IT vendors. It streamlines processes like prior authorization for deeper collaboration.
- Strengthening Standards and APIs
HTI-2 introduces stricter requirements for APIs and mandates the adoption of updated FHIR standards. These changes enable uniformity in data exchange, reducing the fragmentation seen under the roadmap.
- Privacy-Centric Interoperability
HTI-2 incorporates advanced frameworks like SMART on FHIR and OpenID Connect to enhance security while maintaining accessibility. These measures resolve the tension between privacy and usability.
- Patient-Centric Innovations
The rule mandates the use of simplified APIs and tools that empower patients with seamless access to their comprehensive health records addressing usability concerns from the roadmap era.
The Road Ahead with Nalashaa
The CMS Interoperability Roadmap provided a foundation for healthcare data exchange, but its lessons show that the journey might need a little optimization. HTI-2 represents a step forward, leveraging these insights to create a more cohesive, collaborative, and patient-centric healthcare ecosystem.
As the healthcare industry evolves, success will depend on the ability to integrate these lessons into actionable strategies, ensuring interoperability becomes a reality for all stakeholders.
At Nalashaa Solutions, we help healthcare organizations and HIT vendors make informed decisions to combat the complexities of interoperability. From FHIR-based solutions to compliance with evolving regulations like HTI-2, our expertise enables clients to achieve operational efficiency while avoiding costly missteps. Reach out to us at info@nalashaa.com to see how we can make your systems compliant, resilient, and ready for the future of healthcare.