Medication adherence is defined by the World Health Organization as the degree to which the person’s behavior corresponds with the agreed recommendations from a healthcare provider. It includes whether patients take their medications as prescribed as well as whether they continue to take a prescribed medication.
Chief Medical Officer at The Access Group, Dr. Richard G. Stefanacci, stated in one of his studies that payers and providers are spending almost $300 billion in avoidable medical spending due to non-adherence. Payers’ and providers’ losses due to increased hospital readmission for medicare patients is $26 billion per decade. Communication inefficiencies among care providers in U.S. hospitals leading to Non-Adherence cost approximately $12 billion per annum.
It costs billions to pharmaceutical companies in lost business and it is now costing healthcare providers penalties, potentially in the billions, for not achieving accountable outcomes, such as hospital readmission rates, quality payment program (QPP) measures, or effects of the plans’ star ratings under Medicare. Therefore, medical non-adherence is of prime concern in the healthcare industry.
Many of the quality measures in the CMS value purchasing programs are influenced by medication adherence, and some measures capture adherence directly. For example, controlling hypertension and blood sugar—quality measures for MIPS, Advanced APMs for accountable care organizations (ACOs) and Medicare Advantage plans—improves with higher levels of medication adherence.
Types of Non-Adherence
Non-Adherence is categorized as primary, secondary and tertiary in respect to the intensity in which the patient is not adhering to the medication and this is further classified into intentional and unintentional based on the attitude of the patient towards medication.
- Primary Non- Adherence
The patient does not buy the medication which leads to the non-fulfillment of adherence
- Secondary Non-Adherence
The patient does not refill the prescription which is non-persistence adherence
- Tertiary Non-Adherence
The patient fills it but follows an irregular intake of the medication which is non-conforming adherence
Non-adherence mentioned above can be intentional or unintentional
- Intentional non-adherence occurs when there is lack of awareness and the patient refuses to take medication
- Unintentional non-adherence is forgetting due to many reasons including cognitive impairment
Measurement of medication adherence
Adherence is an individual patient behavior. Therefore it should be analyzed and measured keeping the individual in mind. The approaches that have been used for the measurement are:
(1) Subjective measurements obtained by asking patients, family members, caregivers, and physicians about the patient’s medication use
(2) Objective measurements obtained by counting pills, examining pharmacy refill records, or using electronic medication event monitoring systems
(3) Biochemical measurements obtained by adding a nontoxic marker to the medication and detecting its presence in blood or urine or measurement of serum drug levels.
The consequences of non-adherence
From the patients’ perspective, non-adherence results in poor health and financial loss. Non-adherence not only causes waste of medication but also bring about disease progression. Disease progression leads to increased health care cost as disease persists and results in increased use of medical resources such as nursing homes, hospital visits, and hospital admissions. Apart from this, the patient will suffer from reduced functional abilities and a lower quality of life.
Non-Adherence influenced by:
The complexity of treatment regimen which leads to fear and confusion is the primary reason for Non-Adherence. This is endorsed by:
- Patient’s lack of insight into the illness
- Extent, duration of medication and the side effects
- The severity of disease, where the patient develops a lack of belief in the benefit of treatment especially while treating asymptomatic diseases
- Increased cost of medical care
- Patients lack involvement in the treatment decision–making process
- Poor provider-patient relationship
These factors could be tackled by facilitating proper patient-provider communication and educating the patient on the disease and the regime. Apart from the evident factors affecting non-adherence, there are secondary factors which influence the adherence of a patient.
- Cost of medication, copayment, or both
- Psychological problems, especially depression
- Cognitive impairment- Missed appointments
- Inadequate follow-up or discharge planning and office time limitations
- Limited access to care
- Lack of health information technology
Medication adherence is met when:
When the patient has knowledge and clarity on the condition and the purpose of the treatment regime they are more likely to corporate with the medication and treatments. This is further facilitated when:
- The diagnosis and treatment is short-term
- The symptoms are predictable & improve with the medication
- The medication regime is simple and has no or fewer side effects
- The medication is inexpensive
ROLE OF PAYERS AND PROVIDERS
Payers and providers are focusing their attention actively on medication non-adherence as it is costing them time and money by not achieving the desired results with the patients. There are certain areas they are targeting through analyzing the trigger for non-adherence and thereafter to improve medication adherence among the patients. They are listed below:
Triple Aim
The Institute of healthcare improvement (IHI) has developed Triple Aim framework which describes an approach to optimizing health system performance. Through this they intend to:
- Improve the patient experience of care (including quality and satisfaction)
- Improve the health of populations
- Reducing the per capita cost of healthcare.
The IHI is hoping to achieve these benchmarks through planning to redesign the functional structure of Health Care system which includes population health management and system integration and execution.
Patient Centricity
Aims to develop a collaborative and patient-centric accountable care system combining pure technology tools, behavioral modification, and a connected health ecosystem
- Patients are empowered to participate in their own care alternatives
- Healthcare providers are there to support patients and engage in joint decision-making based on individual patient situations
- Getting patient’s insight, input, and connection
Pharmacy Management
Financial constraints play a vital role in promoting medication non-adherence. The high cost of the treatment and medication demotivates the patients from filling or refilling the prescriptions. Thus, by providing financial aid and economic alternatives adherence could be promoted. This could be made possible by:
- Consulting Pharmacy Benefit Managers
- Negotiating drug rebates from manufacturers and discounts from pharmacies
- Promoting generic drug and affordable brand-name medication use
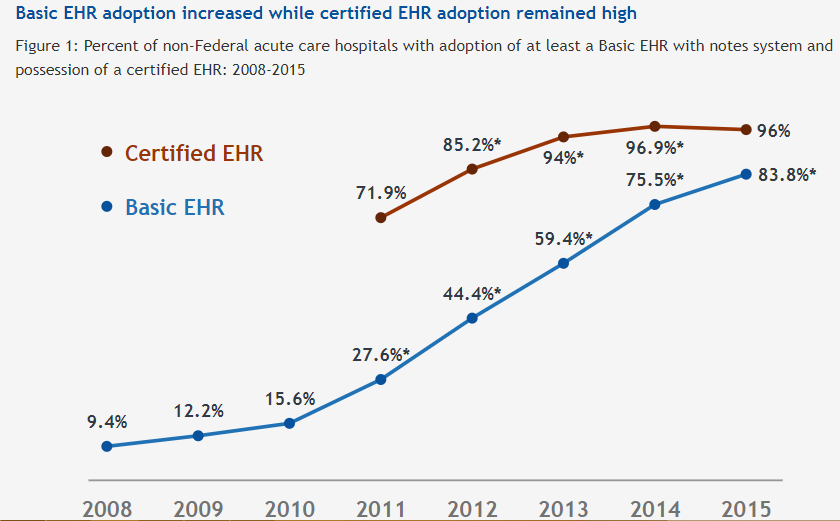
With EHR Incentive Program- 2015 Edition, all the prescribing will need more involvement of the physician and practice by tracking if the medications were filled, changed at the pharmacy and same will be notified to the physician.
Behavioral Coaching
Educating the patient on the importance and the necessity of taking medication on time could help bring down the non-adherence. The patient could be given awareness sessions and doubt clarifying sessions to make an understanding in them about the benefits of taking medication as well as the consequences of not taking medication. If it’s related to cognitive impairment or mental health issues, assistance could be given with the use of technology.
LEVERAGING TECHNOLOGY FOR MEDICAL ADHERENCE
The key to helping patients adhere to treatment plans is to make it easy for them to do so by exploring how patients use technology in everyday life, such as smartphones, tablets, and wearable devices can lend a hand in increasing patient engagement.
Healthcare Apps
Apps are a popular and feasible solution to the problems influencing non-adherence, mostly associated with the busy schedule of everyday life. The advantages of the apps in positively influencing non-adherence are:
- Could be installed on devices like smartphone, tablets and wearable devices like Fitbit
- Interoperability and secure care coordination to enhance clinical communication and workflows where the information could be sent back to the EHR.
- PHI is recorded which gives Medication reminder and information on the patient’s conditions via texts or emails
- Along with reminder, daily snippets to educate the patient on their condition and thus create awareness
Remote Monitoring devices
For patients adamant about not adhering to medication due to behavioral issues or cognitive impairment, getting a third person support could help. Remote monitoring devices could be used to:
- Keep tabs on patients who need to be checked on more frequently than visits allow or are desirable
- Alert system from Bluetooth scales to the case manager
- Interactive voice response to give reminders to take medication as well as to refill the prescription.
- Devices like Blood glucose monitors, activity monitors (such as Fitbit and UP devices), and scales can report back to providers’ electronic medical record systems in order to track patients.
Online Virtual consultation
Convenience plays an important role in facilitating adherence to medication. By promoting and providing an online service where the patient could consult the doctor in their convenience and resolve their doubts related to the health condition or the side effects, it would build confidence in the patient which would promote medication adherence. Other benefits of Virtual consultation are:
- Health insurers offer telemedicine services to help cut costs
- Economic and more convenient for the patients
- Prompt medical attention
- Consult the doctor of choice irrespective of location and time
- Medical history and records are stored online
Implementing EHR and EMR
Awareness and having adequate knowledge can create an impact in solving any problems. Patients tend to disdain medication and treatments due to lack of awareness about the health issue and the purpose of the medication. Also, the inconvenience caused in hospitals from getting an appointment to getting the prescribed medication, causes the patient to ignore the little inconvenience caused by the disease at that point in time. This could be tackled by implementing EHR and EMR which could be useful in ways listed below:
- The increased availability of medication fill histories in clinical practice can provide objective insight into a patient’s medication adherence
- Formulary checking will help physicians prescribe the most-likely-to-be-filled option.
- Electronic prescribing can reduce in-pharmacy wait times
- Reports from the EHR showing refill events, so that gaps in filling maintenance medications can be identified, and those patients can receive active outreach
Pharmacy management Solutions
The objective is not only to make sure the patient buys the medicine but also to verify if the patient is taking them regularly. To motivate them to take the medication, giving them proper information on the medication and facilitating the availability and delivery of the medication is applicable. The aim of pharmacy management software could be as follows:
- Auto refill feature automatically submits a patient’s next refill based on configurable parameters, and can even queue up prescriptions that have no refills for easy viewing and sending out for refill authorization
- A solution where the details of the medication are provided including the purpose, side effects etc. which will give more knowledge about the medication to the patient.
Through expertise in e-Prescribing platforms, Nalashaa intends to give healthcare professionals in all care settings safer and more efficient electronic prescription management, which increases medication adherence and reduces prescription fraud. Through collaboration with healthcare experts’ team, your business will witness improved medication adherence, eliminated manual prescription processes efficiency and improved patient safety.
Riya James
Latest posts by Riya James (see all)
- Proposals in 2020 Payment Notice to reshape ACA Market - January 25, 2019