The Transparency in Coverage (TiC) Rule and the Consolidated Appropriations Act (CAA) were introduced to make healthcare pricing clearer for consumers and employers alike. These regulations require health plans and insurers to publicly share negotiated rates, historical out-of-network costs, and prescription drug pricing, along with real-time cost-sharing estimates through self-service tools and, when requested, on paper.
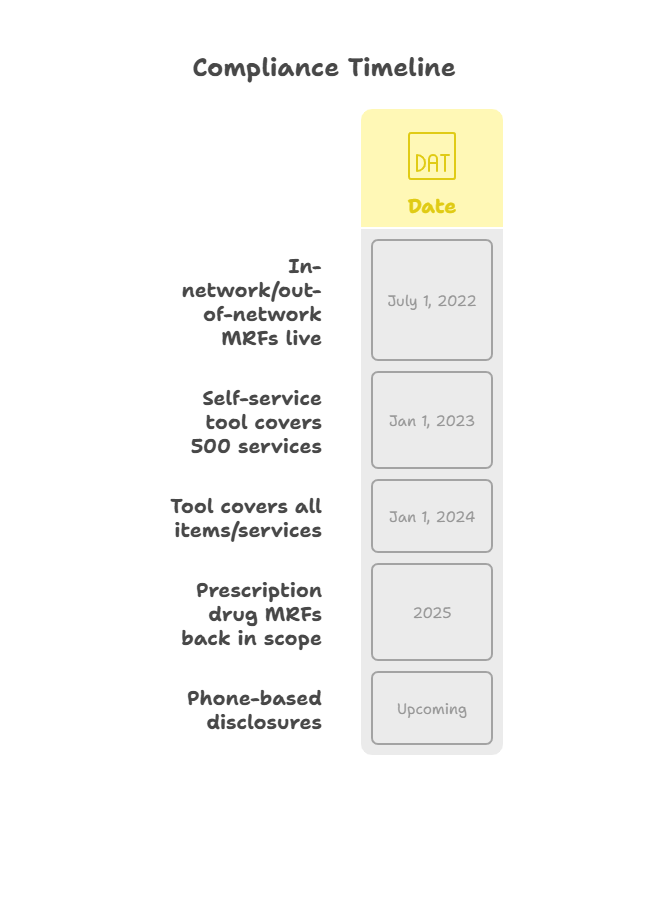
While many requirements took effect as early as 2022, new phases and clarifications continue to emerge. Prescription drug machine-readable files, extended self-service coverage, and updated file standards are among the latest updates payers need to address. Non-compliance can result in penalties and corrective actions, making it critical for health plans to keep processes, data models, and tools aligned with current federal expectations.
This article outlines what the Transparency in Coverage Rule requires today, highlights recent updates for 2025, and explains how payers can maintain compliance without adding unnecessary burden to their internal teams.
Why the Transparency in Coverage Rule Remains Important in 2025
The Transparency in Coverage (TiC) Rule and the Consolidated Appropriations Act (CAA) were introduced to make healthcare pricing clearer for consumers and employers. These regulations require health plans and insurers to publicly share negotiated rates, historical out-of-network costs, and prescription drug pricing, along with real-time cost-sharing estimates through self-service tools and, when requested, on paper.
While many requirements took effect as early as 2022, new phases and clarifications continue to emerge. Prescription drug machine-readable files, extended self-service coverage, and updated file standards are among the latest updates payers need to address. Non-compliance can result in penalties and corrective actions, making it critical for health plans to keep processes, data models, and tools aligned with current federal expectations.
This article outlines what the Transparency in Coverage Rule requires today, highlights recent updates for 2025, and explains how payers can maintain compliance without adding unnecessary burden to their internal teams.
Why the Transparency in Coverage Rule Remains Important in 2025
In 2025, health plans and insurance issuers continue to be responsible for providing clear, accurate pricing and cost-sharing information to plan members and the public. Federal agencies have reinforced that disclosure requirements must be kept current and accessible in multiple formats, including online tools, machine-readable files, and paper on request.
Compliance is not static. Deadlines for self-service tools have expanded to cover all services. Deferred requirements for prescription drug pricing files are now moving forward again. Penalties for non-compliance can include daily fines and additional corrective actions.
Staying aligned with the Transparency in Coverage Rule helps payers meet federal obligations, avoid penalties, and maintain trust with members who rely on accurate estimates when planning care.
Understanding the Transparency in Coverage Rule
The Transparency in Coverage Rule was introduced to make it easier for individuals to access detailed cost and pricing information before receiving care. The rule applies to most group health plans and insurance issuers that offer coverage in the individual and group markets.
Key requirements include:
- Public Machine-Readable Files (MRFs):
Plans must publish files that disclose:
- In-network negotiated rates with providers.
- Historically out-of-network allowed amounts.
- Prescription drug rates and historical net prices.
These files must be updated monthly and made available online in a standard format.
- Internet-Based Self-Service Tool:
Members must be able to use an online tool to view real-time, personalized cost estimates for covered services.
- From January 1, 2023, this tool must cover at least 500 designated shoppable services.
- As of January 1, 2024, the tool must include all covered items and services.
- Paper Form Upon Request:
Cost-sharing estimates must also be provided in paper format if requested by the member.
- Phone-Based Disclosures:
Additional requirements for cost information provided over the phone remain deferred but are under review for future implementation.
Compliance Status and Updates for 2025
Key parts of the Transparency in Coverage Rule are fully in effect, while other elements continue to develop as agencies refine requirements and issue new guidance. As of 2025, health plans and issuers should review the following areas closely:
- Machine-Readable Files:
Publishing in-network negotiated rates and historical out-of-network allowed amounts remains mandatory and must be updated monthly. The requirement for prescription drug pricing files, which was previously delayed, is now back in focus. Many payers may need to coordinate closely with pharmacy benefit managers and data vendors to ensure this information is complete and updated correctly.
- Expanded Self-Service Tool:
The online cost-estimate tool must now cover all covered items and services, not just the initial list of 500 shoppable services. For some plans, extending this functionality to every benefit category requires additional backend updates or closer integration with claims and provider data to keep estimates accurate and usable for members.
- Paper and Telephone Disclosures:
Plans must continue to provide cost-sharing information in paper form upon request. Requirements for providing the same information by phone are still deferred, but organizations should be prepared for possible future implementation, as this may involve additional updates to customer service workflows, call tracking, and audit trail documentation.
- Ongoing Technical Updates:
Agencies continue to request feedback on how to improve the usability and accuracy of machine-readable files, especially for prescription drugs. Payers should expect file format adjustments and potential new technical standards over time, which can add extra review cycles to compliance teams.
Non-compliance can result in civil monetary penalties of up to $100 per day per affected enrollee. Maintaining current files, reliable tools, and clear response processes helps reduce the risk of penalties and operational rework.
Practical Compliance Checklist
Maintaining compliance with the Transparency in Coverage Rule requires clear ownership of tasks, well-structured data processes, and periodic checks to confirm that published information stays accurate and accessible. Below is a practical checklist that health plans and issuers can use to verify readiness:
- Verify Machine-Readable Files (MRFs):
Confirm that in-network negotiated rates and historical out-of-network allowed amounts are published in the required format and updated monthly. Include prescription drug pricing files if applicable, and monitor any new schema updates from federal agencies.
- Review Self-Service Tool Coverage:
Ensure the internet-based cost-sharing tool includes all covered items and services, not just the initial list of shoppable services. Test for real-time estimate accuracy and ease of use.
- Maintain Paper Disclosure Process:
Check that cost-sharing estimates are available in paper form when requested and that staff are trained to handle these requests promptly.
- Prepare for Phone-Based Requests:
While the phone disclosure requirement remains deferred, it may be activated in future updates. Review whether current customer service systems can track call logs and document audit trails if needed.
- Monitor Gag Clause Provisions:
Review provider and vendor contracts to confirm that gag clauses prohibiting disclosure of price or quality information are removed, as required by the Consolidated Appropriations Act.
- Track Regulatory Updates:
Designate internal resources or external partners to follow new guidance, Requests for Information (RFIs), or clarifications that may adjust file structures, reporting formats, or deadlines.
- Plan for Internal Audits:
Schedule periodic checks to confirm that published files match internal rate agreements and that tools deliver reliable estimates to members.
A clear, repeatable checklist can help reduce last-minute compliance issues and limit the risk of penalties or corrective actions.
Why Payers Should Maintain Compliance Continuously
Meeting the requirements of the Transparency in Coverage Rule is not a one-time project. As federal guidance evolves, payers are expected to keep pricing data current, maintain accurate estimates, and respond promptly to member requests for information in different formats.
Regular compliance checks help reduce the risk of civil penalties and unexpected rework when audits or inquiries occur. For many organizations, clear cost information also supports other business priorities, such as strengthening member trust, demonstrating plan value to employers, and reducing instances of unexpected medical bills.
Staying current with transparency rules can also help health plans position themselves more competitively. Well-maintained public files and reliable estimate tools make it easier for members and employers to compare plan performance and understand out-of-pocket costs before services are delivered.
How Nalashaa Supports Payers with Compliance
Maintaining ongoing compliance with the Transparency in Coverage Rule and related requirements under the Consolidated Appropriations Act can involve significant data handling, system updates, and process oversight. Nalashaa works with payers to help manage this workload through tailored technology and support services.
Our teams assist with:
- Machine-Readable File Management: Structuring, publishing, and updating in-network, out-of-network, and prescription drug files in line with federal guidelines.
- Self-Service Tool Enhancements: Developing or refining online cost estimate tools to cover all required services with real-time accuracy.
- Data Integration: Connecting multiple data sources, including pharmacy benefit managers and provider contracts, to keep pricing data reliable and consistent.
- Workflow Updates: Preparing internal systems to manage paper-based disclosures and planning for future phone-based requests if activated.
- Contract Reviews: Helping identify potential gag clauses and supporting compliance with related CAA provisions.
- Continuous Monitoring: Providing technical updates and support as new rule changes, RFIs, or clarifications are released.
Consistent monitoring, clear responsibilities, and strong technical support can help payers manage updates without disrupting internal teams or member services.
Navigating updates and maintaining compliance does not need to overwhelm internal teams. Nalashaa’s Healthcare Compliance Services help payers manage file structures, cost-estimate tools, data integrations, and related system changes with confidence.
For questions or to discuss a tailored approach to compliance, connect with us at info@nalashaa.com
Latest posts by Priti Prabha (see all)
- ONC HTI 1 Final Rule and Certified APIs: A Complete Guide - February 19, 2026