1. What is USCDI?
USCDI is the government’s way of saying: “Here’s the basic health data everyone should be able to share.”
Short for United States Core Data for Interoperability, USCDI is a standardized list of patient data points that electronic health systems must support for exchange. It includes essential fields like allergies, medications, procedures, and clinical notes—things you’d expect to be consistent no matter where you go for care.
The initiative comes from the 21st Century Cures Act, which set a clear goal: make it easier for health data to move freely and securely across systems. USCDI is one of the rulebooks that ensures everyone, EHR vendors, app developers, hospitals, and public health systems, play by the same data-sharing rules.
2. How USCDI Makes Interoperability Work
Interoperability sounds great in theory: your health data should follow you wherever you go. But in practice, systems don’t always agree on what “health data” means—or how it should be formatted.
That’s where USCDI comes in. It sets the baseline for what data must be shared and how it should be labeled. So, when one system sends over a patient’s vitals or lab results, the receiving system knows exactly what to expect, no guesswork, no custom mappings.
USCDI works hand-in-hand with FHIR, the modern API standard for exchanging health data. Together, they ensure that the right information moves between systems in real-time, with fewer errors and fewer delays.
3. What’s Included in USCDI?
USCDI is a curated set of data that the healthcare system agrees is essential to exchange. Whether you’re switching providers, moving to a new state, or syncing your health data with an app, these are the data points that should follow you.
Each version of USCDI organizes this information into data classes, which are broad categories, and data elements, which are the individual fields within those categories.
Here’s a closer look at what USCDI typically includes:
| Data Class | Sample Data Elements |
| Demographics | First name, last name, date of birth, race, ethnicity, preferred language |
| Vital Signs | Blood pressure, heart rate, height, weight, body temperature |
| Laboratory | Blood pressure, heart rate, height, weight, and body temperature |
| Medications | Medication name, dosage, route, frequency, prescribing provider |
| Allergies & Intolerances | Substance, reaction type, severity, onset date |
| Immunizations | Vaccine name, date administered, manufacturer, lot number |
| Clinical Notes | Progress notes, consultation notes, discharge summaries, history & physicals |
| Procedures | Procedure name, date, performing provider |
| Care Team Members | Names, roles, and contact info of clinicians involved in a patient’s care |
| Problems | Diagnoses, onset/resolution dates, SNOMED/ICD codes |
| Smoking Status | Current, former, or never smoker |
Each of these elements is defined so that different systems use the same labels, structures, and meanings. That way, when data is exchanged, it’s not just readable—it’s usable.
4. Understanding the Different USCDI Versions (V1 to V5)
Healthcare keeps evolving, and so does USCDI. Each new version adds data that reflects emerging priorities—whether that’s equity, mental health, or more personalized care. Here’s a clearer look at what changed across the versions:
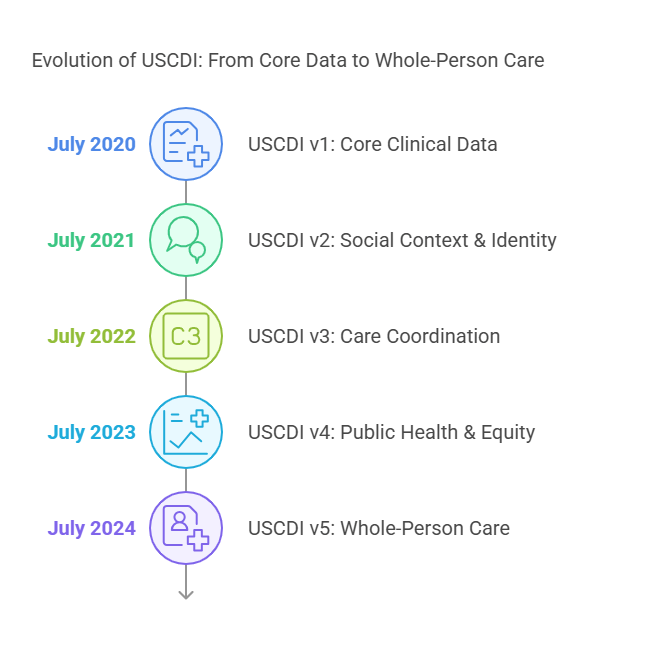
USCDI v1 – Released 2020
This was the starting line. It pulled together data from prior programs like Meaningful Use and the Common Clinical Data Set (CCDS).
- Covered essential clinical data like demographics, allergies, meds, lab results, and vital signs
- Included clinical notes, making it easier to understand the context behind structured data
- Became the minimum dataset required for EHR certification under the Cures Act
USCDI v2 – Released 2021
USCDI v2 brought social and demographic depth.
- Added sexual orientation and gender identity (SOGI) fields
- Introduced social history to account for external influences on health
- Expanded patient identifiers to improve matching and record integrity
- Aligned more closely with efforts to reduce care disparities
USCDI v3 – Released 2022
This version emphasized care coordination and status tracking.
- Introduced disability status, functional status, and mental/cognitive function
- Expanded care team information—roles, contacts, organizations
- Improved address fields for better patient matching across systems
- Supported value-based care models by adding more outcomes-related data
USCDI v4 – Released 2023
In this version focus shifted to public health reporting and equity.
- Added diagnostic imaging data, supporting broader clinical documentation
- Introduced health insurance information—critical for administrative workflows
- Strengthened representation for substance use data
- Enhanced data element definitions to improve clarity and consistency
USCDI v5 – Released 2024
This is the most forward-looking version so far, anticipating future regulatory needs.
- Added reproductive health data (e.g., pregnancy status, fertility information)
- Included behavioral health assessments and screening tools
- Introduced communication preferences to support patient-centered care
- Designed to better align with FHIR-based APIs and rules under HTI-2
5. USCDI and FHIR: What’s the Connection?
To understand how USCDI fits into the bigger interoperability picture, you need to know about FHIR—Fast Healthcare Interoperability Resources.
FHIR is a set of rules and standards developed by HL7 to help health data move between systems using APIs (the same technology behind most modern apps). It lets developers build tools that connect with EHRs and health data platforms in real time, without needing to hard-code integrations for each vendor.
So, where does USCDI come in?
USCDI defines what data should be exchanged. FHIR defines how to exchange it.
Let’s say a patient schedules an appointment through a telehealth platform. The platform needs access to their medications, lab results, and allergies. Using a FHIR API, the app can pull that data directly from the patient’s EHR. But what fields should it ask for? What labels and formats should it expect? That’s where USCDI steps in. It ensures both systems agree on the structure and content of that data.
Why This Matters
Without USCDI, different systems might refer to the same field in different ways. One EHR might label a medication as “current meds,” another as “active prescriptions.” FHIR alone won’t solve that. But FHIR with USCDI ensures that when data moves, it’s in the right format, and meaning is preserved.
This combination also plays a huge role in the Information Blocking Rule from the Cures Act. Under that rule, certified health IT developers are required to support FHIR APIs that allow patients and third-party apps to access their health information, and that information must conform to the USCDI standard.
In short:
- USCDI = standardized content
- FHIR = standardized transport mechanism
Together, they form the technical backbone of modern healthcare data exchange.
6. Who Needs to Comply with USCDI and Why?
USCDI isn’t a “nice to have”—it’s required for many players in the healthcare space, especially those dealing with certified health IT. Here’s a breakdown of who’s affected and what’s at stake:
Health IT Vendors and Developers
If you build software for healthcare—whether it’s an EHR system, a patient portal, or a telehealth app—you likely fall under ONC’s certification program. That means your software must be able to support the latest version of USCDI through standardized APIs (often FHIR-based).
Failing to keep up with USCDI updates can put your certification at risk, which in turn makes it harder to sell your product to providers who rely on certified solutions.
EHR Developers and Implementers
EHR vendors are on the front lines of USCDI compliance. They have to support each new version and make sure the implementation aligns with federal requirements. This includes:
- Accurately mapping fields to USCDI-defined data elements
- Supporting FHIR APIs for access and exchange
- Documenting how the system handles USCDI data
If USCDI elements are poorly integrated, it could lead to incomplete data transfers or patient safety issues.
Healthcare Providers Using Certified Health IT
While providers aren’t usually the ones building APIs, they’re directly affected. If their EHR doesn’t comply with USCDI, they may:
- Be out of alignment with CMS and ONC requirements
- Risk non-compliance with information blocking rules
- Miss out on interoperability incentives under programs like MIPS or Promoting Interoperability
In practical terms, USCDI compliance means smoother referrals, better coordination with external specialists, and fewer blind spots in patient history.
Why It Matters
The industry is moving away from siloed systems and toward data liquidity. USCDI is central to that transition. Whether you’re building a solution or using one, aligning with USCDI isn’t just about compliance—it’s about staying relevant in a healthcare system that expects data to move easily, accurately, and securely.
7. Common Challenges with USCDI Adoption
While the idea behind USCDI is simple—define what data should be shared—implementing it isn’t always straightforward. For many healthcare organizations and IT vendors, adoption comes with a few practical hurdles.
EHR Limitations
Most EHRs weren’t built with USCDI in mind. Older systems may lack the flexibility to support new data elements, especially when those fields don’t map cleanly to existing database structures. Adding support for fields like gender identity or social history might require not just UI changes, but a backend redesign.
And when EHRs aren’t equipped to handle the latest version, providers are left with partial compliance at best—or fragmented data at worst.
Mapping Legacy Data to USCDI Formats
Even if a system can support USCDI, it doesn’t mean the data already inside it is clean or standardized. Older systems often use proprietary codes, custom fields, or inconsistent terminology. Mapping those to USCDI-defined elements takes time, manual review, and often a fair bit of guesswork.
This is especially tricky for organizations with years of historical data that was never collected or labeled with structured interoperability in mind.
Keeping Up with Changing Versions
Each version of USCDI introduces new data elements, and those changes aren’t optional. For vendors trying to stay certified and for providers trying to remain compliant, this means tracking the latest version, understanding what’s new, and updating systems accordingly.
These updates often come with short timelines and complex documentation, leaving teams scrambling to implement changes without disrupting workflows.
Integrating USCDI with Existing Systems
USCDI has to work with other data standards, custom APIs, and business logic already in place. Integrating it into a live system—without breaking something else—can be a major challenge.
It’s not just about adding new fields. It’s about syncing those fields across care teams, billing systems, patient portals, mobile apps, and more. And that level of integration takes careful planning, testing, and coordination across departments.
8. Benefits of USCDI in Real-Life Healthcare Settings
Despite the challenges, the payoff for adopting USCDI is real and growing. When implemented well, it creates a better experience not just for systems, but for people.
Faster Patient Record Exchange
Information moves faster when systems agree on what data to send and how to send it. Instead of waiting on faxed records or re-entering data manually, providers can access the details they need instantly, from vitals to imaging results, all in a standardized format.
This matters most during transitions of care, where delays or missing data can directly affect outcomes.
More Coordinated Care Across Providers
Primary care, specialists, labs, pharmacies—they all use different systems. USCDI gives them a shared language. This means fewer blind spots, fewer redundant tests, and better coordination across settings.
When everyone sees the same medication list or problem history, care becomes more connected—and less reactive.
Improved Data Accuracy and Patient Matching
One of the less obvious but critical benefits of USCDI is better data integrity. Standardized formats and consistent data elements make it easier to match patient records across organizations. This reduces the risk of duplicate charts, fragmented histories, or missing allergies—errors that could impact care quality or patient safety.
Foundation for Public Health Reporting and Analytics
USCDI doesn’t just help providers—it helps systems understand populations. With consistent data fields across organizations, public health agencies and research teams can aggregate data more accurately. That makes it easier to spot trends, track outbreaks, analyze equity gaps, and shape policy.
It also enables cleaner inputs for AI and predictive analytics, which depend heavily on standardized, structured data.’
Conclusion: Making Data Exchange Work, One Standard at a Time
USCDI plays a quiet but critical role in modern healthcare. It doesn’t deliver care, schedule appointments, or manage claims—but it ensures that the systems behind all those tasks can communicate. It sets the foundation for consistent, secure, and accurate health data exchange, whether between providers, across states, or into a patient’s smartphone app.
For HIT vendors, it’s no longer enough to just support EHR functionality. Systems need to be interoperable by design, and that starts with keeping up with USCDI and its evolving versions. For healthcare providers, it’s a chance to improve the continuity of care, reduce friction between systems, and eliminate the common headaches caused by inconsistent data.
That said, staying compliant with USCDI—while managing system upgrades, legacy data, and real-time integration—can be complex.
At Nalashaa, we work with HIT vendors, EHR developers, and healthcare organizations to bridge technical gaps and bring systems up to modern interoperability standards. Whether it’s mapping legacy records to USCDI fields, building FHIR APIs for data exchange, or preparing your systems for future versions, our team offers the depth of expertise and flexibility that evolving compliance demands.
Need help navigating USCDI and the broader compliance landscape?
Let’s make interoperability work for you with our Healthcare Interoperability Solutions. Connect with us at info@nalashaa.com
FAQs
1. What’s the difference between USCDI and FHIR?
USCDI defines what data should be exchanged—things like medications, allergies, lab results—using a standardized set of fields.
FHIR, on the other hand, defines how that data is exchanged using APIs. Think of USCDI as the content, and FHIR as the delivery method.
2. Is USCDI mandatory?
Yes, for certified health IT developers. Under the 21st Century Cures Act, systems certified by the ONC must support the current version of USCDI for data exchange, especially via FHIR APIs. It’s also a key part of complying with information blocking regulations.
3. What is the purpose of USCDI?
USCDI exists to make sure health data can be shared across different systems in a consistent, accurate, and structured way. It helps clinicians, software vendors, and healthcare organizations speak the same data language, whether for patient care, public health, or analytics.
4. What are data standards in interoperability?
Data standards make it possible for systems to understand the data they exchange. They support semantic interoperability, which means that different systems can interpret the data in the same way. For example, one system might say “Tylenol” while another says “acetaminophen”—standards ensure both are recognized as the same thing.
5. How often is USCDI updated?
USCDI is updated approximately once a year. Each version introduces new data classes or elements based on stakeholder feedback, healthcare priorities, and evolving regulatory requirements.
6. How can vendors prepare for upcoming USCDI versions?
Vendors can stay ahead by:
- Monitoring ONC’s official USCDI updates
- Reviewing draft versions early
- Assessing system readiness for new data classes
- Collaborating with clinical stakeholders to validate mappings
- Aligning their FHIR APIs to support added fields
Preparing early reduces the rush to meet compliance deadlines and helps ensure smooth integration into existing workflows.