Healthcare organizations are facing pressure on two fronts: regulatory deadlines and cybersecurity fallout. CMS now requires prior authorization decisions to be delivered within 72 hours for urgent cases, using FHIR-based APIs. This changes how payers and providers exchange data, making traditional batch-file systems a liability.
At the same time, the Change Healthcare cyberattack in early 2024 exposed claims and billing data for nearly 190 million people. It was the largest healthcare data breach to date and a clear warning that fragmented systems create risk.
Together, these forces are making one thing clear. Disconnected systems and siloed workflows no longer work. Whether it’s authorizations, claims, or eligibility, healthcare data must be integrated, fast, and secure. In 2025, real-time, standards-driven healthcare data integration is foundational.
2. What Healthcare Data Integration Means in 2025
Healthcare data integration in 2025 goes beyond merging files or syncing databases. It’s about creating fast, secure, and consistent data flow between clinical, claims, billing, eligibility, and provider systems. Information moves in real time, without manual uploads or disconnected systems slowing things down.
Three core pillars define modern healthcare data integration:
FHIR R4 and Bulk FHIR as the foundation
FHIR (Fast Healthcare Interoperability Resources) enables systems to exchange structured health records, such as demographics, medications, encounters, and authorizations, using efficient APIs. It replaces older document-based formats with standardized, modular data exchange.
TEFCA’s national “network of networks” model
The Trusted Exchange Framework and Common Agreement (TEFCA) sets technical and legal standards for secure data sharing across Qualified Health Information Networks (QHINs). With version 2.1, FHIR-based exchanges are the default, making it easier for organizations to connect without one-off contracts.
Event-driven APIs and streaming data pipelines
Instead of relying on batch uploads, many systems are shifting to streaming architectures. These allow for real-time updates for claims status, eligibility checks, and prior authorizations, keeping all systems in sync with minimal delay.
Together, these pillars support a faster, more connected healthcare environment where data is available when and where it’s needed.
3. Regulatory Tailwinds You Can’t Ignore
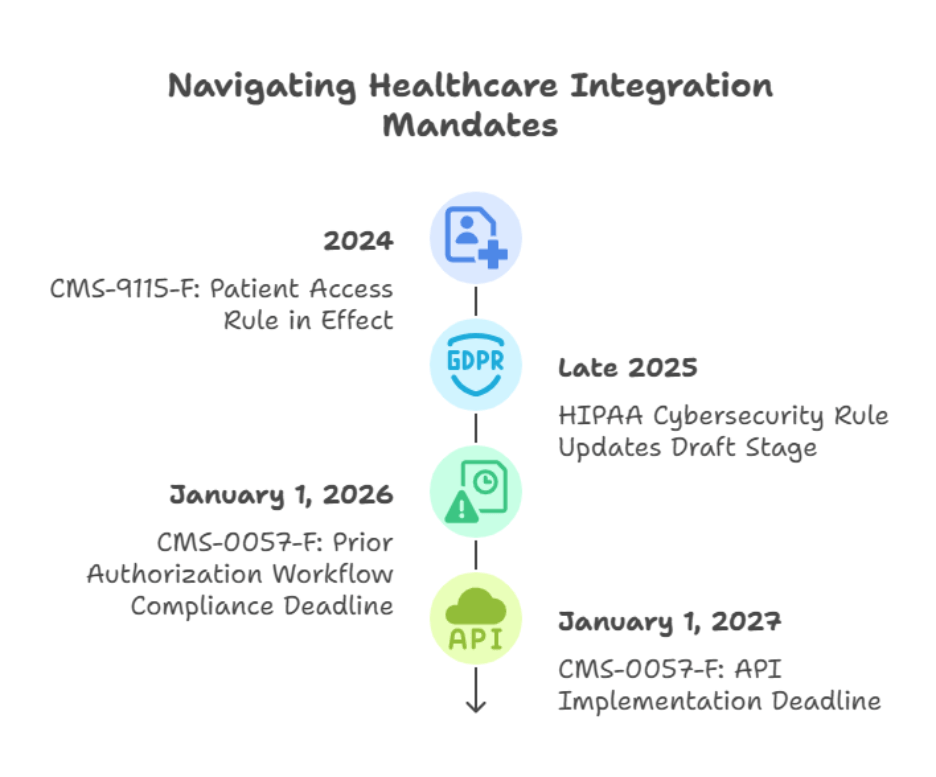
Healthcare data integration is no longer driven by innovation alone. Federal mandates are now pushing payers and providers to modernize how they exchange information. Three major rules are shaping the pace and direction of change.
CMS-0057-F: Prior Authorization Rule
This rule requires payers to respond to urgent prior authorization requests within 72 hours and standard requests within seven calendar days. It mandates the use of FHIR APIs for submitting, checking, and tracking prior authorizations. The rule also introduces clear reporting requirements to increase transparency and reduce administrative friction.
Why it matters: Manual prior authorization processes are no longer viable. Real-time data integration with EHRs and payer systems is essential.
Key deadlines:
- January 1, 2026, for workflow compliance
- January 1, 2027, for API implementation
CMS-9115-F: Patient Access Rule
This rule mandates that payers make claims and encounter data available to members through secure, standardized APIs. It builds on the original 2020 version and reinforces the need for data to be accessible, portable, and up to date.
Why it matters: Members expect seamless digital access to their health data. Any delays or gaps due to siloed systems damage trust and increase churn risk.
HIPAA and Cybersecurity Modernization
In response to the 2024 Change Healthcare breach, HHS is drafting stronger security rules for healthcare data exchange. The new guidance includes stricter audit trails, zero trust principles, and breach response planning. While final rules are still in development, they reflect a shift in how health data security will be enforced going forward.
Why it matters: Integration is not just about convenience; it now directly affects compliance and organizational risk exposure.
4. High-Impact Benefits for Payers
Here’s how healthcare data integration delivers real value for payers, backed by current industry insights:
- Streamlined Operations and Faster Processing
Integrated workflows consolidate eligibility, claims, billing, and authorization timelines into one cohesive process. This reduces manual handoffs and accelerates adjudication, often cutting processing cycles by up to 30–50% while minimizing errors.
- Sharper Insights for Risk and Analytics
When payer systems unify clinical, claims, and financial data, analytics engines can deliver accurate risk scoring and identify care gaps early. Leading AI models trained on that integrated data reduce overpayments and improve cost predictions by up to 20%, particularly for complex, high-cost patients.
- Better Fraud and Payment Integrity Performance
Real-time access combined with integrated datasets helps detect anomalies such as duplicate claims or upcoding before any payment occurs. That proactively guards against overruns and saves on post-pay audit costs.
- Improved Member Experience and Retention
Members value fast, transparent interactions that integrated data enables, like up-to-date eligibility checks and instant EOB access. Submit inquiries and notifications seamlessly, reducing inbound customer service issues and boosting satisfaction.
- Stronger Data-Driven Business Strategy
Clean, unified data provides the backbone for value-based contract modeling, product innovation, and network expansion. Payers investing in integration are better positioned to roll out new care pathways and personalized offerings.
- Cost Savings and Resource Optimization
Reducing redundancy and automating manual data workflows delivers operational savings. Teams can shift focus to proactive analytics rather than data entry, increasing bandwidth for high-value tasks.
5. High-Impact Benefits for Providers
Here’s how strong healthcare data integration helps providers, backed by real-world insights and industry trends from 2025:
- More Accurate Clinical Decisions
When clinical data, lab results, billing, and claims are unified, doctors get a complete patient snapshot. That means fewer duplicative tests, better diagnosis, and personalized care plans. Integration lays the groundwork for decision support tools that reduce medical errors.
- Fewer Claims Denials and Faster Payments
With clean data passing through eligibility and payer edits before submission, providers see fewer coding mismatches or missing authorizations. That means higher first-pass acceptance and steadier cash flow.
- Operational Efficiency and Lower Administrative Costs
Joined-up systems cut administrative friction. Appointment schedules, billing, and documentation sync automatically, eliminating manual reconciliations and email or phone delays. Staff can then focus on patient care, not paperwork.
- Compliance Made Easier
Integrated systems support easier extraction and reporting for quality frameworks like MIPS, HEDIS, UDS, or accreditation requirements. The right data is automatically tagged and available for audits or regulator reviews.
- Stronger Care Coordination
Real-time access to encounter data, referral status, and authorization lists helps care teams work more smoothly across departments and facilities. That improves transitions of care, reduces readmissions, and enhances patient outcomes.
- Better Use of Advanced Analytics and AI
Providers with integrated datasets can leverage AI for predictive care, flagging high-risk patients, optimizing bed management, and prioritizing clinical attention. As AI-driven healthcare tools expand in 2025, clean data becomes indispensable.
6. Technology Enablers Driving the Shift
To support real-time collaboration between payers and providers, healthcare organizations are leaning into a new tech stack built for speed, interoperability, and security. These tools replace aging, fragmented systems with smarter, more connected infrastructure.
FHIR APIs and SMART on FHIR Apps
FHIR (Fast Healthcare Interoperability Resources) is the interoperability standard that healthcare systems now depend on. Built on modern web protocols like REST and HTTP, it enables structured data exchange in JSON or XML formats. This approach replaces legacy HL7 and flat-file systems with modular, resource-oriented APIs for everything from patient demographics to authorizations. SMART on FHIR builds on FHIR to deliver secure, user-friendly clinician and patient apps that plug into EHRs. No-code platforms such as DrapCode have democratized app creation across these protocols.
FHIR-Based Data Lakes and Mesh Architectures
Healthcare systems are now aggregating streaming data from EHR events, lab integrations, wearable devices, and claims into real-time data lakes. This creates a foundation for scalable analytics and predictive models such as readmission risk and sepsis alerts. A data mesh ensures governance remains decentralized. These setups let users trigger dashboards and interventions based on live data feeds.
Low-Code / No-Code Integration Platforms
Platforms like eZintegrations™, Goldfinch AI, DrapCode, and others let organizations connect existing systems quickly—without starting from scratch. These platforms support both file-based ingestion and FHIR APIs, standardizing data and simplifying mapping. They enable faster ROI and allow clinical or operations teams to own integration logic directly.
Event-Driven Streaming and Real-Time Pipelines
Traditional batch windows are being replaced with event-based data flows that notify systems immediately of eligibility changes, authorization updates, or claim events. Streaming platforms, such as Kafka-style message buses, keep all systems synchronized with low latency and high reliability.
AI/ML Services for Data Quality and Insights
Machine learning is being applied to cleaning, normalizing, and deduplicating data at ingest. NLP can extract structured elements from unstructured clinical notes or referrals. Graph analytics detect fraudulent patterns across claims and provider networks, while predictive models enable pre-emptive care—flagging high-risk profiles before costs escalate.
Zero Trust Security and Compliance Architecture
A zero-trust model treats every user, device, and data flow as untrusted until explicitly verified. It includes mutual TLS, multi-factor authentication, adaptive access controls, micro-segmentation, and continuous audit logging. This design aligns directly with HIPAA and evolving CMS guidance, strengthening both security and compliance.
7. Readiness Checklist
Before investing in or expanding your healthcare data integration strategy, it’s important to assess where your organization stands. These five questions can help surface gaps in your current systems and guide your next steps:
- Can we surface a member’s claim, authorization, or eligibility status in under 30 seconds?
If the answer requires multiple logins or batch processing, your systems are not integrated in real time.
- Are our systems capable of sending and receiving FHIR R4 resources today?
Many organizations claim FHIR compatibility but still rely on custom formats or outdated standards.
- Do we apply data quality checks before information enters downstream systems?
Cleansing, deduplication, and standardization should happen at the point of data intake, not after the fact.
- Are our fraud detection and risk models using unified data from claims, clinical, and billing sources?
Siloed inputs lead to blind spots. Integrated data makes pattern recognition more accurate and timely.
- Have we mapped out which legacy systems still need to be wrapped or replaced?
If key workflows depend on flat files or unsupported platforms, those should be on a phased retirement plan.
Conclusion
Healthcare data integration is no longer a future goal. It’s now a regulatory requirement, a security priority, and a competitive advantage. Whether you’re trying to meet CMS mandates, prevent the next ransomware disaster, or reduce costly inefficiencies, fragmented systems will hold you back.
At Nalashaa Health, we work with payers and providers to build fast, secure, standards-based data pipelines that connect the full care and revenue lifecycle. Our team can help you implement FHIR APIs, integrate legacy systems, and enable real-time insights across your organization.
If your data exchange workflows are overdue for an upgrade, start by exploring our Healthcare Data Integration Services. Or reach out directly at info@nalashaa.com to discuss where you are today and where you want to be.