Home health agencies can now report the costs of Remote Patient Monitoring (RPM) services to Medicare for Reimbursement. The latest update to the 2019 Physician Fee Schedule, the RPM reimbursement final rule introduces vital changes in the form of new CPT codes, vastly improving the prospects for telehealth technology.
In 2017, the Centre for Medicare and Medicaid Services (CMS) published a two-year study that demonstrated adequately how an increase in patient awareness and the close monitoring of patient awareness saved millions of dollars for Medicare. This study was an important part of the Chronic Care Management (CCM) program and it helped the CMS realize the importance of Remote Patient Monitoring (RPM) for the first time.
In 2018, the CMS went on to create designated provisions for remote patient monitoring reimbursement with the release of CPT code 99091. This enabled care providers to receive payment for the “collection and interpretation of physiologic data”. Despite the strong start, CPT 99091 did not consider the costs of equipment set up and the effort required to train patients on the program involving the devices.
The biggest downside of this initiative was that it required care providers to interact with patients for at least 30 minutes on a daily basis for 30 days.
The Focussed Effort From the CMS
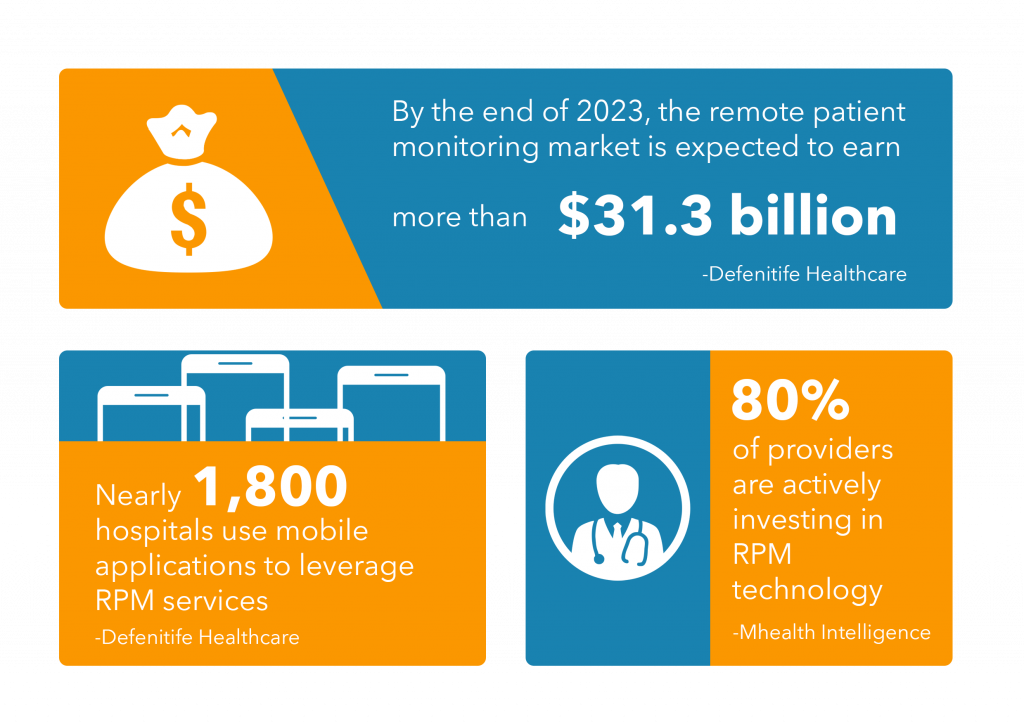
It didn’t take long for the CMS to realize the shortcomings of this first initiative to reimburse care providers for RPM services. The following statistics made the perfect case for CMS to explore the advantages of RPM services.
This is why in the final rule on Chronic Care Remote Physiologic Monitoring introduces three new CPT codes to cover the costs involved in the set up of medical devices as well.
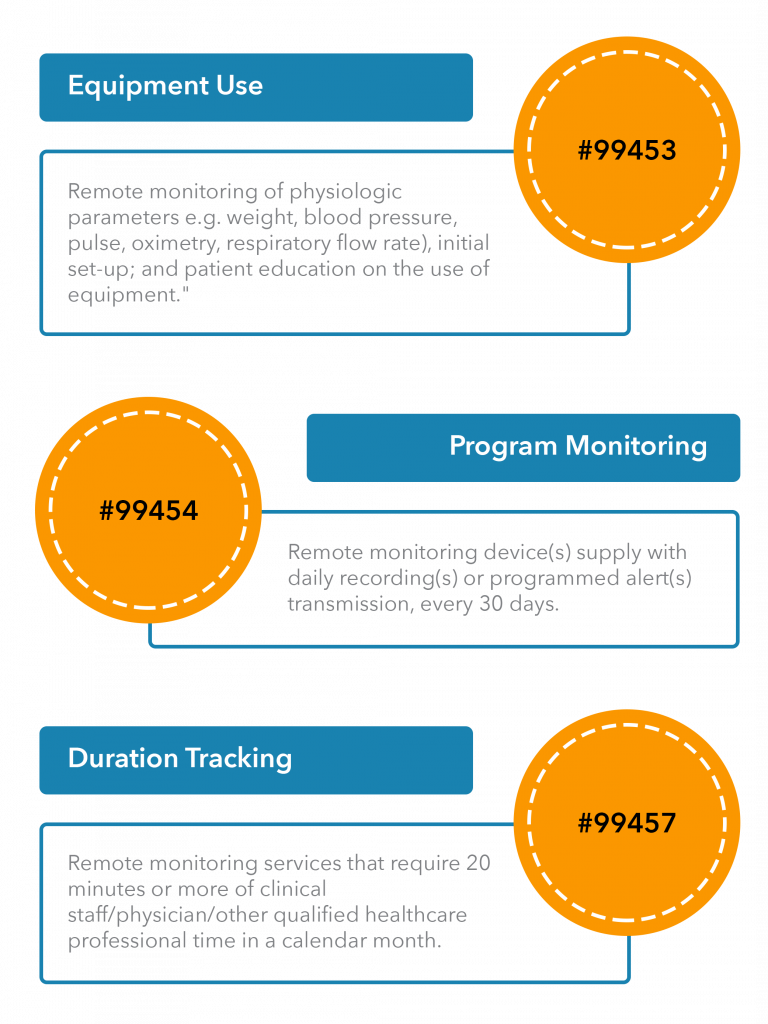
Here is an overview of the new CPT codes:
CMS Reimbursement Requirements
While the final rule on remote patient monitoring reimbursement is long and descriptive, it does not cover the technology use cases under the new CPT codes in detail. The CMS has been asked to elaborate on the released CPT codes by covering reimbursement slabs for the use of healthcare technologies to monitor patients. This process is bound to use up the first half of 2020.
The immediate focus of RPM service providers and hospitals must be on the requirements that qualify them for CMS reimbursements for using RPM services. The following are the criteria to qualify for reimbursement:
- Medicare Part B patients are charged a 20 per cent copayment (routinely waiving copays can trigger fines under the federal Civil Monetary Penalties Law and the Anti-Kickback Statute).
- Patients opt-in for remote monitoring services.
- The service is ordered by a physician or other qualified healthcare professional” (such as a nurse practitioner, certified nurse specialist or physician assistant).
- Data can be wirelessly synced for evaluation.
- Patients are monitored for at least 16 days to be applied to a billing period.
The sustained efforts of the CMS and its intent to facilitate the digital transformation seem to have arrived at the right time. Hospitals that were overwhelmed with reducing rehospitalization and home health agencies that needed incentives for using something both easily accessible and effective as RPM stand to gain the most.
Before the initiative from the CMS to promote the regular use of RPM services, care providers and home health agencies had no choice but to pass the burden of costs on the patient. The new reimbursement model gives both RPM service providers and patients some relief from increasing costs, originating from equipment management and installation costs.
Conclusion
The RPM final rule encourages home health agencies and PAC providers to leverage proven technology to improve the care process. Providers now have an effective way of reducing Instances of rehospitalization by tracking patient health meticulously without the concern of escalating costs.
To explore the potential of RPM services, care providers need to be invested in technology. Nalashaa’s diverse experience in the design and development of healthcare IT solutions may be a great place, to begin with.
To know more about our healthcare product engineering services, drop us a line at info@nalashaa.com.