As patient expectations rise and the healthcare landscape grows more connected, one question remains: Why is interoperability so important in healthcare? Whether you’re a hospital administrator worried about data silos, a clinician seeking faster, more accurate insights, or an IT leader preparing for tomorrow’s regulatory demands, the push for seamless data exchange has never been more urgent.
Interoperability fuels everything from robust medication safety measures to better-coordinated care, sitting at the core of modern healthcare’s transformation. We’ll explain why interoperable systems are vital, illustrate how they can elevate care delivery, and offer guidance on overcoming the most common roadblocks.
What is Healthcare Interoperability?
Healthcare interoperability is the ability of different health information systems, devices, and applications to seamlessly access, exchange, integrate, and cooperatively use data in a coordinated manner. According to the Office of the National Coordinator for Health Information Technology (ONC), interoperability ensures that health information is readily available and can be understood and acted upon when and where it’s needed. This capability goes beyond merely sending data back and forth—it’s about making that information meaningful and actionable across various platforms.
“Interoperability is the ability of two or more systems to exchange health information and use the information once it is received.”
— Office of the National Coordinator for Health IT (ONC)
When systems are interoperable, clinicians can quickly view a patient’s medical history from another facility, administrative teams avoid duplicative tasks, and ultimately, patients benefit from a more coordinated, efficient care experience.
Types of Interoperability
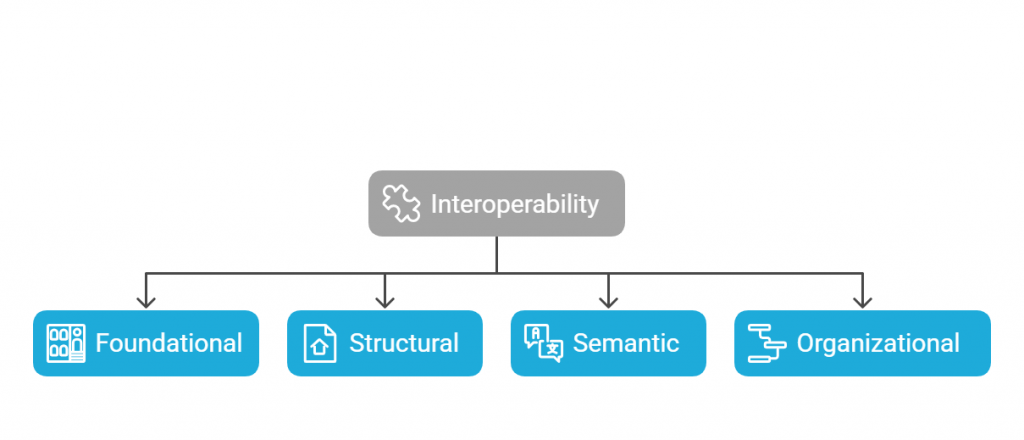
Most industry frameworks break interoperability down into four primary layers. Each layer represents a step toward more comprehensive and meaningful data exchange:
- Foundational (Data Exchange)
- What It Is: The basic capacity for one system to send and receive data from another.
- Example: A patient’s lab results are transmitted from a standalone lab system to a hospital’s EHR, even if the hospital can’t automatically interpret the data’s meaning.
- Structural (Data Format)
- What It Is: The uniform arrangement of data exchange. This ensures that data fields and formats are consistent across systems.
- Example: Using standard message formats like HL7 v2 or FHIR for lab results, enabling a lab system and an EHR to “speak the same language” structurally.
- Semantic (Shared Interpretation)
- What It Is: The ability of different systems to interpret and use the data they receive in a meaningful way.
- Example: A medication list is transmitted from one EHR to another, where both systems not only receive the medication codes (e.g., SNOMED CT) but also recognize them as the same drug, dosage, and frequency, so clinicians see a coherent medication profile.
- Organizational (Processes & Governance)
- What It Is: The policies, procedures, governance models, and social frameworks that enable secure and efficient data sharing across entire networks of providers.
- Example: A regional Health Information Exchange (HIE) or a Trusted Exchange Framework (TEFCA) environment where multiple stakeholders—hospitals, clinics, labs, and payers—agree on rules for data sharing, consent, and privacy.
These layers involve consistent standards, strong data governance, and a commitment to collaborative workflows.
Why Is Interoperability Important in Healthcare?
The layers of interoperability—foundational, structural, semantic, and organization empower healthcare organizations at every level, from frontline clinicians making quick decisions to executives shaping long-term strategies. Here are a few key dimensions that highlight its critical role:
- Elevating Patient Care & Outcomes
When disparate systems talk to each other, clinicians gain immediate access to a patient’s comprehensive medical history, current medications, and lab results, reducing the risk of errors and missing information. A more holistic view of the patient’s data means more accurate diagnoses and smoother care coordination.
- Regulatory Compliance & Incentives
Regulatory initiatives such as the 21st Century Cures Act and guidelines from the Office of the National Coordinator (ONC) explicitly push for seamless data sharing. HIPAA also emphasizes secure but fluid information flow. Interoperability avoids potential penalties and also unlocks the benefits of value-based care programs.
- Reducing Administrative Burden
Interoperable systems minimize repetitive tasks and redundant data entry. Rather than manually re-entering patient details or reconciling conflicting records, administrative staff can focus on higher-value activities. This efficiency often translates into lower operational costs, improved patient throughput, and fewer billing errors—all of which support the organization’s bottom line.
Benefits of Healthcare Interoperability
Integrated systems drive a transformation that goes beyond simple data sharing. Here, we explore how enhanced connectivity creates tangible improvements across the healthcare spectrum.
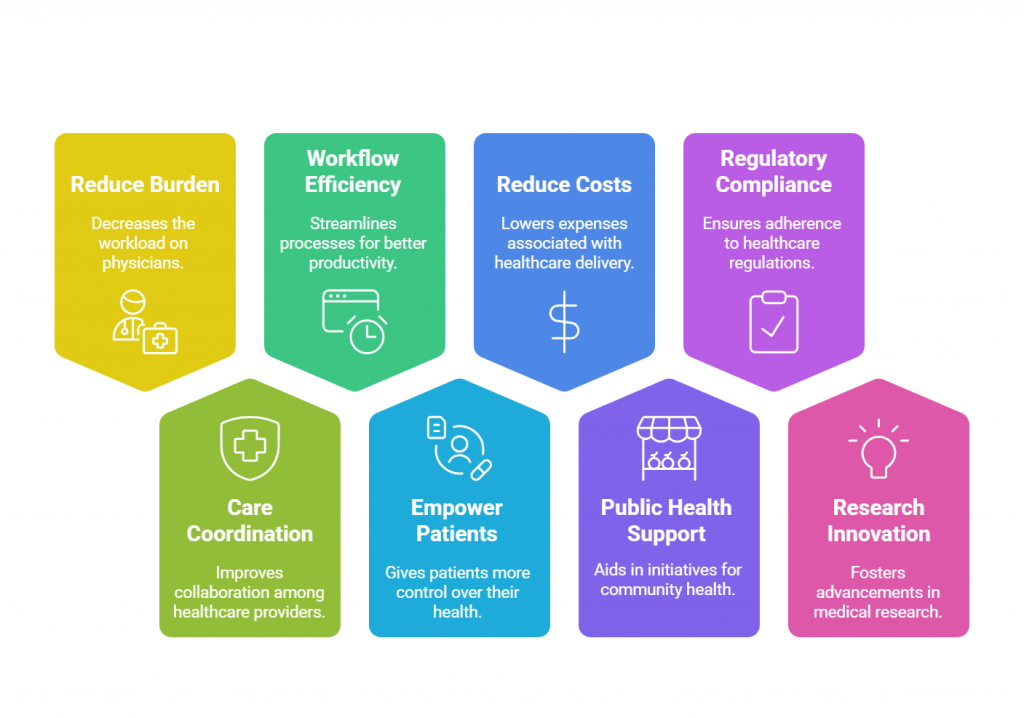
Reduce Physician Burden
Modern EHR solutions pool data from multiple sources, cutting down on tedious manual entry and letting physicians concentrate on care. At the same time, intelligent filtering tools prevent information overload by highlighting only the most relevant patient details, easing the clinical workflow, and mitigating burnout.
Enhance Care Coordination
When care teams share the same up-to-date patient data, unnecessary tests and conflicting treatment plans diminish. Whether a patient is referred to a specialist or transitions between facilities, their information follows them, ensuring seamless communication.
Improve Workflow Efficiency
Interoperability streamlines both clinical and administrative processes by eliminating duplicate work. Providers can make faster decisions, and patients enjoy convenient features like online scheduling and portal access. Reduced paperwork also means lower operational costs, aligning with healthcare’s push toward efficiency.
Empower Patients
When people can view their lab results, medications, and care plans in real-time, they become active participants in their health. Regulatory requirements like the Patient Access Final Rule further accelerate this shift, compelling payers to share patient data more openly and securely.
Reduce Costs
Better data sharing leads to fewer hospital readmissions, minimized duplicate tests, and more targeted treatments—all of which lower expenses. On the administrative side, automating billing and pharmacy workflows drives down overhead, helping organizations operate more sustainably.
Support Public Health Initiatives
Shared data helps officials spot outbreaks, allocate resources, and develop targeted interventions more quickly. With electronic case reporting and aggregated records, health agencies can track population health trends accurately, reducing manual reporting errors and delays.
Advanced Research and Innovation
Robust interoperability opens the door to more diverse data sets for clinical trials and medical research. Integrating real-world data from wearables and remote monitoring can accelerate drug development, refine treatment protocols, and drive meaningful healthcare advancements.
Meet Regulatory Requirements
As laws like the 21st Century Cures Act mandate better data sharing, adopting interoperable systems ensures compliance and positions organizations to benefit from patient-focused initiatives. It also aligns with global efforts, such as Canada’s Interoperability Roadmap, to standardize and streamline healthcare information exchange.
How Interoperability Impacts Healthcare Delivery
In healthcare, every second matters. Let’s see how.
Speed of Information Sharing
One of the most immediate effects of interoperability on healthcare delivery is the rapid exchange of patient data across systems. Instead of waiting for faxes or manually re-entering information, clinicians and administrative teams can access up-to-date records in near real-time. This accelerates decision-making and cuts down on administrative overheads.
Emergency Situations
When every second counts, the ability to instantly retrieve patient histories, allergies, and medication lists can be lifesaving. Interoperable systems ensure that first responders and emergency department teams have immediate visibility into a patient’s critical details. This reduces the risk of adverse events, speeds up treatment, and fosters an environment where clinical staff can focus on patient stabilization rather than data gathering.
Care Settings Diversity
Interoperability isn’t confined to a single setting; it supports care continuity across outpatient clinics, inpatient wards, behavioral health programs, and post-acute facilities. Real-time data sharing means a specialist can review a primary care doctor’s note before a referral appointment or a rehabilitation center can update hospital staff on a patient’s progress. By connecting these diverse settings, interoperability makes it easier to coordinate treatment plans, track recovery milestones, and maintain a unified record of a patient’s health journey.
Examples of Interoperability in Healthcare
EHR-to-HIE Integration
A prime example is a hospital system that links its Electronic Health Records to a statewide Health Information Exchange (HIE). By automatically sending and receiving patient data through the HIE, authorized providers can instantly review past diagnoses, recent imaging, and care notes, regardless of where the patient was treated. This level of connectivity not only reduces duplicative testing but also streamlines transitions between different care settings.
Laboratory & Pharmacy Systems
Another common scenario involves lab and pharmacy integrations. Instead of manually faxing lab reports or pharmacy orders, results and prescriptions flow electronically into the provider’s EHR. By bypassing paper-based processes, clinicians receive real-time updates, patients get faster test outcomes, and pharmacies can process medications promptly, minimizing wait times and potential errors.
Patient Wearables & Remote Monitoring
With more patients using health-tracking devices, interoperability allows wearable data, such as heart rate, blood glucose, or sleep patterns, to feed directly into the clinical record. Providers can spot early warning signs, adjust treatment plans proactively, and engage patients in self-management. This continuous data loop is especially beneficial for those with chronic conditions who require close monitoring over time.
Cross-Platform Telehealth Solutions
Telehealth platforms that sync seamlessly with EHRs and remote monitoring tools give clinicians a complete view of a patient’s status during virtual visits. Whether the consultation is for routine follow-up or urgent care, practitioners can access the latest vitals, lab results, and specialist notes, ensuring remote services meet the same standard of care as in-person appointments.
Radiology & Imaging Systems
When Radiology Information Systems (RIS) or Picture Archiving and Communication Systems (PACS) connect seamlessly with a hospital’s EHR, clinicians can quickly view X-rays, MRIs, and CT scans from within the patient’s electronic record. This integration not only accelerates the diagnostic process but also eliminates the need for multiple logins and reduces the risk of misplacing critical images.
Immunization Registries
In many regions, healthcare providers automatically share vaccination data with state or national immunization registries. These interoperable connections ensure that public health agencies have real-time insight into vaccination rates and patients can maintain a single, centralized record, helpful for everything from school enrollment to travel requirements.
Payer & Claims Integration
Some EHR systems directly interface with insurance platforms, allowing automatic transmission of claims data. This bidirectional flow reduces paperwork, speeds up reimbursement, and cuts down on billing errors, creating a smoother experience for both healthcare providers and patients.
Behavioral & Mental Health Services
By linking mental health providers with primary care teams through secure data exchange, interoperability ensures that treatment plans, therapy notes, and medication updates are incorporated into a patient’s overall health record. This comprehensive view promotes coordinated, stigma-free care and helps clinicians address both physical and mental health needs holistically.
Medical Device Integration
In critical care settings, interoperable monitors and infusion pumps can feed real-time vitals and dosage information into the EHR. Nurses and physicians benefit from immediate updates and fewer data entry tasks, improving accuracy while freeing clinicians to devote more attention to direct patient care.
7. Best Practices to Achieve Seamless Interoperability
Creating a truly connected healthcare ecosystem calls for thoughtful collaboration and ongoing support. The key best practices to make interoperability a reality are:
Adopt Recognized Standards
Building interoperability on widely accepted frameworks like HL7, FHIR, and TEFCA helps different systems “speak” a common language. Standardized data formats, APIs, and protocols ensure that the information exchanged is accurate, secure, and usable across diverse platforms and providers.
Invest in Scalable Infrastructure
Cloud-based solutions, robust APIs, and flexible architecture are vital for managing the growing volume and complexity of healthcare data. As organizations expand or adopt new technologies, such as AI-driven diagnostics or remote monitoring devices, they need infrastructure that can evolve without compromising performance.
Engage Stakeholders Early
Interoperability affects everyone, from clinicians and administrators to IT teams and patients. By involving these groups in decision-making from the start, you’re more likely to design solutions that align with actual workflows, regulatory requirements, and patient needs. Early stakeholder buy-in also reduces resistance to change.
Continuous Training & Support
No matter how advanced your systems are, they’ll only be effective if people know how to use them. Providing ongoing education, user-friendly interfaces, and accessible help resources encourages adoption and helps staff gain the confidence to leverage interoperability.
Conclusion
Achieving true interoperability isn’t just a checkbox—it’s an investment in healthcare’s future. From expedited patient care and reduced administrative burdens to better research capabilities and stronger public health initiatives, interoperable systems have the power to transform every layer of healthcare delivery. By adopting recognized standards, prioritizing scalable infrastructure, and actively involving your stakeholders, you can create a seamless data environment that benefits both providers and patients.
Ready to take the next step? Explore our Healthcare Interoperability Solutions to learn how we can help you design, implement, and optimize a secure, connected infrastructure. Whether you’re seeking a demo, a consultation, or a comprehensive whitepaper, our experts are here to guide you. Let’s work together to build a smarter, more collaborative healthcare ecosystem.