RPA – A short overview
Robotic Process Automation (RPA) is a technology that allows businesses to automate routine and repetitive tasks using software robots, or “bots”. These bots mimic human actions to interact with digital systems and perform tasks such as data entry, processing transactions, and managing records. RPA is designed to streamline operations, reduce errors, and increase efficiency by freeing up human employees to focus on more strategic work.
RPA in Healthcare RCM
Many key aspects of the healthcare revenue cycle have been driven by manual processes that are borderline monotonous. Let’s face it; healthcare providers are having to ‘do more with less’ due to changing healthcare regulations, and much-needed respite is long overdue. In short, the current need of the hour for healthcare providers is effective billing and tracking procedures to ensure an uninterrupted flow of revenue.
If you are reading this and if you are leading a team of RCM experts, you are already aware of the cold hard truth:
Hospitals and health systems must ensure reimbursement is collected properly and timely, to remain fiscally viable.
In this publication, we cover the causes and solutions to overcome this friction in healthcare revenue cycle automation through Robotic Process Automation (RPA), an essential component of RCM healthcare services.
Related: The Areas of Automation in Healthcare
So What’s the Difficulty with Healthcare Revenue Cycle Management Anyway?
Healthcare providers require RCM teams with a detailed knowledge of treatment and reimbursement guidelines to manage the process. Unfortunately, despite being competent, they are significantly prone to errors in data entry due to the volume and variety of data they are required to scrutinize. Simple problems like errors in data entry are exacerbating the struggle of practice leaders.
The shocking part is that the conundrums hounding healthcare revenue cycle management have been at it for many decades and practice leaders appear to be ok with dragging them along as deadweight!
Are you having trouble maintaining your revenue cycle?
So Where’s the Reprieve?
The ‘diagnosis’ for the healthcare revenue cycle problems lies in understanding the problems arising from its various functions. This must be followed by understanding how automation can plug into the process flow without disrupting it.
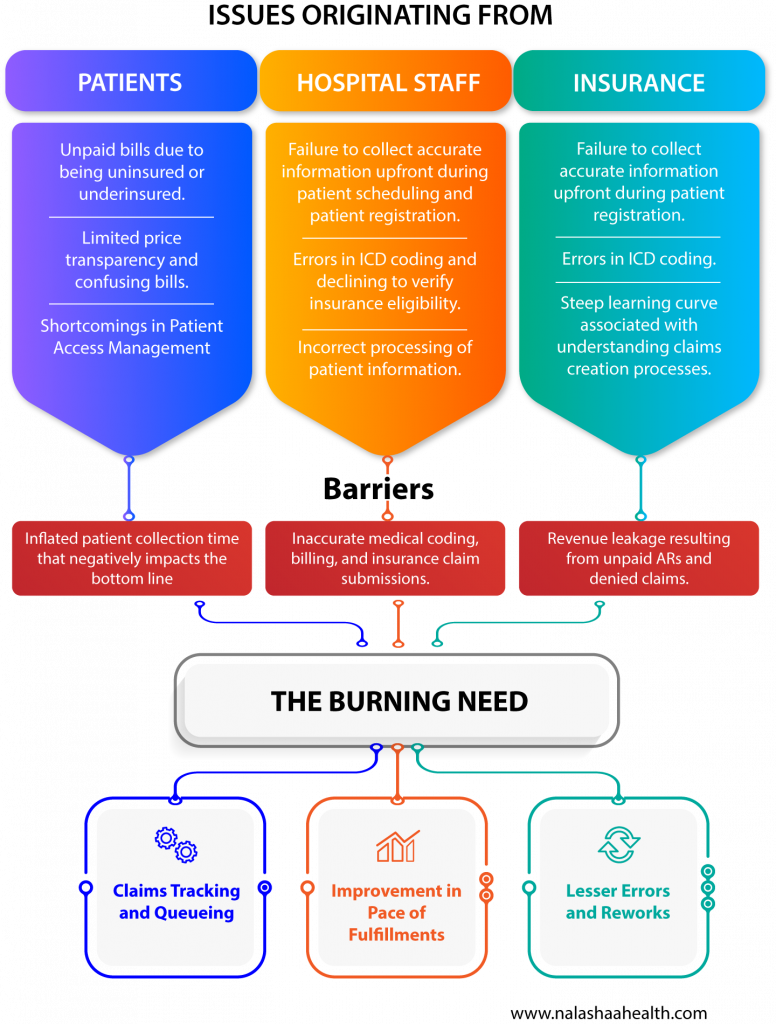
The diagram below shows the current challenges in the healthcare revenue cycle and the intervention required from RCM experts.
We can help you break the barriers with automation
And how does RPA in Healthcare Ease the Difficulty of Revenue Cycle Management in Healthcare?
Before we delve deeper, it’s crucial to recognize that RPA isn’t a cure-all for challenges in healthcare revenue cycle management (RCM). Nonetheless, it is a powerful tool to automate specific processes within the healthcare revenue cycle. By integrating RPA, healthcare organizations can expect to see significant reductions in costs and processing times.
Here are the five high-impact areas for revenue cycle automation in healthcare and the results A/R experts can expect.
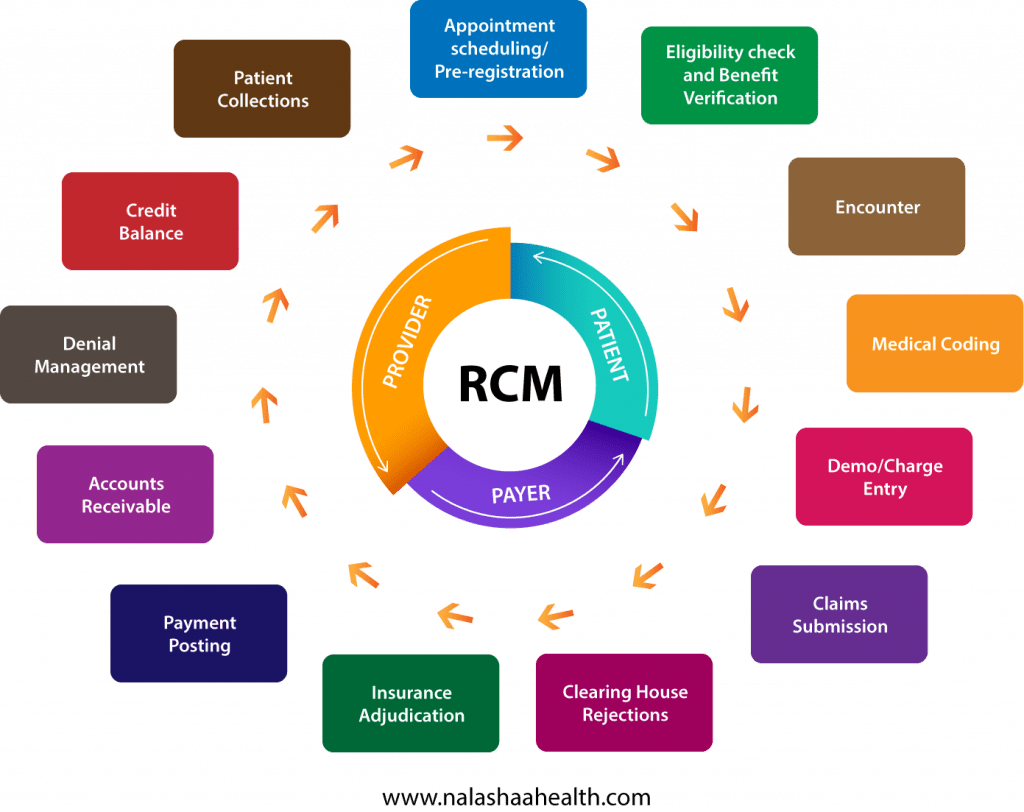
1. Eligibility Check and Benefit Verification:
Prior Authorization: RPA bots can navigate to the eligibility check section of payer portals to gather information to submit a prior authorization request. It can then open a list of patients who require an eligibility check and perform the process by selecting one patient at a time.
Patient Data Updating: Bots can populate data spreadsheets with vital information such as Management Minutes Category Code (MMC Code) to determine reimbursement amounts. It accurately records the appropriate reimbursement amount to be awarded to providers using the standard reimbursement facility rates data on payer portals.
Document Preparation for Review: Upon completing the eligibility check, RPA bots can consolidate a record of all the patients scrutinized for submission to the billing supervisor.
Expected Outcomes: RPA bots are capable of running 500+ records per day, reducing the propensity of denied claims by 70%.
2. Medical Billing:
Data Export: RPA bots retrieve accounts receivable data from care providers’ practice management systems using filters such as the ‘time in the queue’. They can then log into payer portals and retrieve claim status for specific claims.
Managing No-Response Claims: Effective and continuous follow-up is the only solution for claims that go unanswered by payer organizations. RPA bots can filter claims that match the criteria for ‘no response’ and regularly alert A/R specialists for further escalation.
Expected Outcomes: RPA bots can eliminate the need to manually check for claims status by upto 25 minutes per inquiry. Providers can expect the reduction of manual efforts in the checking of no-response claims by 23%.
3. Charge Entry
Review of Superbills: RPA Bots download superbills containing all the patient visit and clinical encounter information and primes them for review by the medical coding team. It also extrapolates and aligns data with the practice management system during the charge submission process.
Charge Submission: Bots are configured to specifically address the process flow of healthcare practices and ensure the accurate compilation and submission of charges for claims processing.
Expected Outcomes: Reduced errors in data entry and reduction of Full Time Equivalent (FTE) or employee scheduled hours by 40% in the charge entry process.
4. Payment Posting
ERA Posting: RPA bots can log into clearinghouses and payer websites to download and analyze the Electronic Remittance Advice or ERA. Bots can then complete the electronic posting of the completed ERAs.
Validation and Error Checks: RPA bots can also perform a follow-up quality check step that involves validating ERA files to ensure there are no errors in the patient treatment details mentioned in the ERA document.
Expected Outcomes: Upto 25% expense reductions in the ERA cash posting process.
5. Denial Management
The Exception Flow: Besides assisting with the prevention of denied claims, RPA bots also offer significant support for A/R specialists in denial management. Bots move claims that cannot be salvaged to an exception path flow where A/R specialists can move them to a high-priority manual intervention and correction queue.
Pattern Detection: RPA Bots can ‘track’ and highlight error patterns in the claims denial management process. The analysis highlighted by RPA bots enables A/R specialists to make effective/corrective changes to the claims submission process.
Related: Reimagining Claims Status Check and Payment Posting processes with automation
All Aboard the Healthcare Revenue Cycle Automation Bandwagon?
With over 10 years of experience in healthcare software development, at Nalashaa, we recommend a cautious but steady approach to the adoption of RPA for your healthcare practice. The ideal approach would be to plug in RPA based on your area of specialization. Specific guidelines to enhance reimbursements with RPA that would yield a greater ROI and unlock opportunities for further improvement.
Send us an email at info@nalashaa.com to know how you can customize the power and potential of RPA to the specific needs of your healthcare practice.
Puneeth Salian
Latest posts by Puneeth Salian (see all)
- Top 10 EHR Implementation Strategies for Vendors - July 23, 2024