From member enrollment, eligibility checks, and provider network management to billing and collection, healthcare payers are involved in handling and reporting sensitive healthcare data. The healthcare payer process is drawn out and cumbersome, with human errors resulting in penalties and loss of revenue, and must be automated at all costs. Besides the obvious benefits of report automation, it provides an excellent opportunity for all external stakeholders to view and analyze data efficiently in a customized manner.

Payer Challenges in Absence of Report Automation
Traditionally, payers were all about generating reports on an ad-hoc basis. A dedicated team would produce reports based on requests from the senior management.
Payers face unavoidable roadblocks with manual reporting, such as:
Cost Inefficiency
- Payers deal with copious amounts of data. Incorrect data add a fair margin of human errors, resulting in inaccurate reports and hence revenue loss.
- Inaccurate manual reporting leads to flawed business goals, implying higher expenditure and weaker ROI.
Time–Consuming Tasks
- Manual creation of reports involving healthcare data, such as claims, billings, credentialing, and inventory and supply chain management is a tedious process.
- Manually creating reports from large pools of data leaves the workforce with little time to focus on other core areas.
Data Inaccuracy
- Payers indulge in several data processing workflows, from code entry to eligibility, and claim management, with high possibilities of data inaccuracies.
- Erroneous reports could result in ineffective strategies for the payer organization.
Security Concerns
- Human error is the leading cause of healthcare data breaches. Creating healthcare reports containing sensitive data manually adds to the chances of such breaches.
- Human negligence in healthcare reporting could land payers in violation of security clauses in compliances such as HIPAA, SOX, and GLBA.
Eliminate the above-outlined mistakes by automating the reporting process. Report automation, be it in enrollment, credentialing, billing, or records management, ensures that a payer organization stays ahead of the competition by providing a smooth and streamlined experience to its members, providers, and hospitals.
Automated Reporting to the Rescue
It is essential to first understand the reporting requirements of the organization, like the frequency of reports, the medium of reporting, etc.
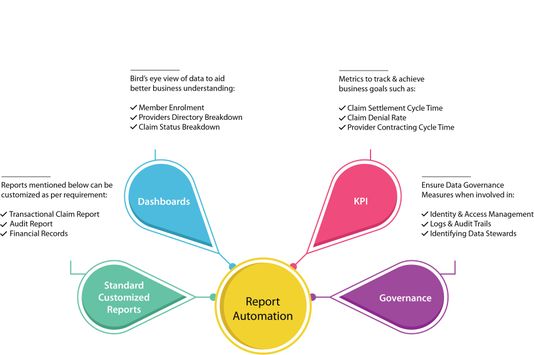
Based on the business use cases, the payer organizations should use appropriate reporting and data visualization tools to create standard and customized reports, as and when required. Digital reporting solutions can be used to generate interactive visuals, charts, or maps if required.
New generation tools like Tableau, Power BI, and Cognos give better control to users to fetch and visualize data in the desired format.
Benefits of Employing Report Automation
Automation of reports helps organizations to create a secure environment by restricting data access on a need-to-know basis. Moreover, report automation comes with a plethora of other benefits that make the user’s life easy.
Reduced Cost with Increasing Efficiency
- Automating claims, billing, inventory, and supply chain management reports cut down on the need for resources, reducing the overhead costs.
- Reduced human intervention increases the efficiency of teams and allows for better business decisions.
Increased Data Quality
- With automated reporting, the space for human negligence, be it in billing or claim denials, is minimal to zero.
- Report automation carries out quality checks to ensure that data management is streamlined and that the data quality is high.
Flexibility in Data Visualization
- With report automation tools in place, payer organizations can customize standardized reports such as traditional claim reports, audit reports, and financial records.
- Data visualization allows for a clear understanding of reports and helps users to identify trends quickly.
Zero Breach of Compliance
- With report automation tools, breach of security clauses of regulations laid out by the US Department of Health and Human Services (HHS) is unlikely.
- Report automation helps in adhering to security compliance requirements such as SOX, NIST, PCI DSS.
Focus on Core Areas
- Report automation allows the payer to focus on areas that need human attention, be it reasons for rejected claims or claim fraud, and improve those areas.
- Users can share selected KPIs from within these reports with external and internal stakeholders through visualized dashboards.
With report automation in the picture, payer organizations can focus better on human-centric tasks and process optimization. Due to individual interactions with reporting tools, auditing would also be straight forward.
Count on Your Technology Partner
With deep experience in interactive & advanced data dashboards, automation partners can help their clients to derive actionable insights for optimum results.
Connect with our experts at Nalashaa and accomplish your business goals efficiently by setting up report automation and a compliant analytics culture.
Reach out to us at info@nalashaa.com.